Cardiology
Session: Cardiology 1
148 - Speckle Strain Assessment of Left Atrial Function in Pediatric Patients with Normal Functioning Bicuspid Aortic Valve
Monday, May 6, 2024
9:30 AM - 11:30 AM ET
Poster Number: 148
Publication Number: 148.2731
Publication Number: 148.2731
- SA
Sanjeev Aggarwal, MD
Professor of Pediatrics, Division of Pediatric Cardiology
Children's Hospital of Michigan
Detroit, Michigan, United States
Presenting Author(s)
Background: Bicuspid aortic valve (BAV) can be associated with ascending aortic dilation due to intrinsic wall abnormalities of the aorta or mechanical forces. Abnormalities in the ascending aorta may lead to increase in afterload on the left ventricle (LV) that may, in turn, impair the LV function. Recently, left atrial (LA) speckle strain has been used as an early marker of LV diastolic dysfunction. However, the phenotype of LA functional profile of a normal functioning BAV is lacking.
Objective: To compare the LA strain parameters of normal functioning BAV with those of normal controls.
Design/Methods: Retrospective chart and echocardiogram (ECHO) reviews of patients who had diagnoses of BAV without significant aortic valve stenosis or regurgitation were performed. Patients with coarctation or ventricular septal defect repair or abnormal LV systolic function were excluded. Patients who presented to our cardiology clinic with chest pain, murmur, or syncope and had normal ECHOs acted as normal controls. Using vendor independent software (TomTec Imaging, Inc.), a single observer blinded to clinical data measured LA strain. One full cardiac cycle with zero strain reference was set at RR on EKG. The 3 phases of LA strain curve, a) reservoir phase (LASr) denoting atrial filling, b) conduit phase (LAScd) representing passive emptying and c) booster phase (LASct) representing active atrial contraction were measured. Similarly, the largest LA volumes (LAESV) and minimal LA volumes (LAEDV) were measured. LASr < 27 is taken as abnormal, based on published norms. Student t-test (SPSS Inc.) was used for comparisons and p< 0.05 was considered significant.
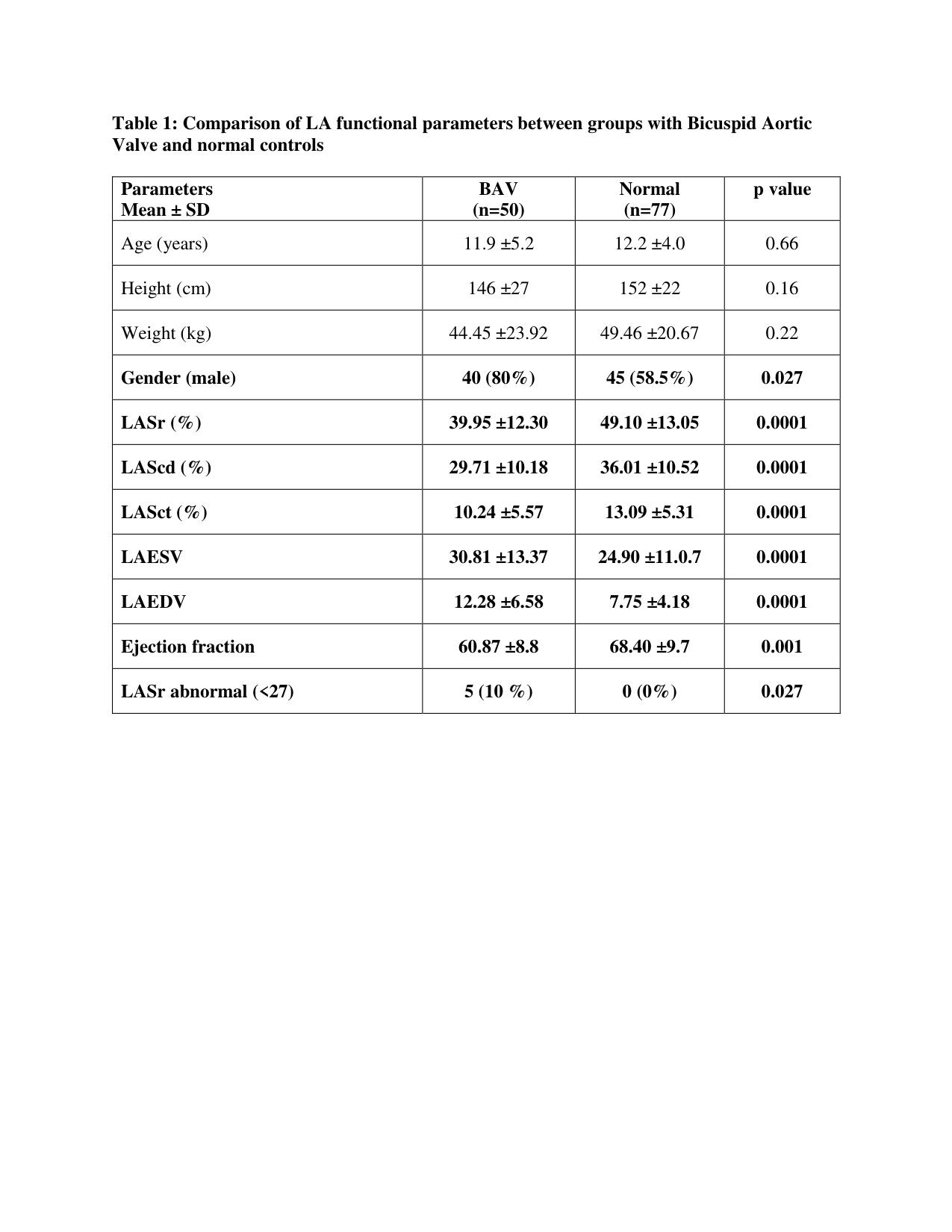
Results: Our cohort consisted of 50 patients with mean (SD) age of 11.9 (5.2) years, 40 (80%) were male. The BAV and normal (n=77) groups were similar in demographic data except for the preponderance of males in BAV as expected. LASr, the primary LA functional parameter was significantly lower (39.95 ±12.30 vs. 49.10 ±13.05, p= 0.0001) and LA was significantly dilated in both systole and diastole in the BAV group, compared to normal. Around 10% of patients with BAV had abnormal LASr.
Conclusion(s): Our data shows a novel profile of LA functional anomalies in children with BAV even with no significant stenosis or regurgitation. This is an intriguing finding, which we speculate may be explained by altered afterload related to intrinsic aortic wall abnormalities even in the presence of normal functioning BAV. Further longitudinal examination of LA function on speckle tracking imaging is warranted in children with BAV.