Adolescent Medicine
Session: Adolescent Medicine 2
153 - Characteristics of Receiving HPV Vaccine since 2019: A Quality Improvement Project
Friday, May 3, 2024
5:15 PM - 7:15 PM ET
Poster Number: 153
Publication Number: 153.599
Publication Number: 153.599

Jenny Francis, MD, MPH (she/her/hers)
Associate Professor
University of Texas Southwestern Medical School
Dallas, Texas, United States
Presenting Author(s)
Background: Human papillomavirus (HPV) is a common sexually transmitted infection known to cause various types of cancer and genital warts. HPV vaccines can be administered at age nine years to ensure protection prior to HPV exposure and reduce the burden of future HPV-related diseases.
Objective: Characterize HPV vaccination prevalence among 9-to-22-year-olds in one academic primary care center from 2019-2022 during quality improvement interventions.
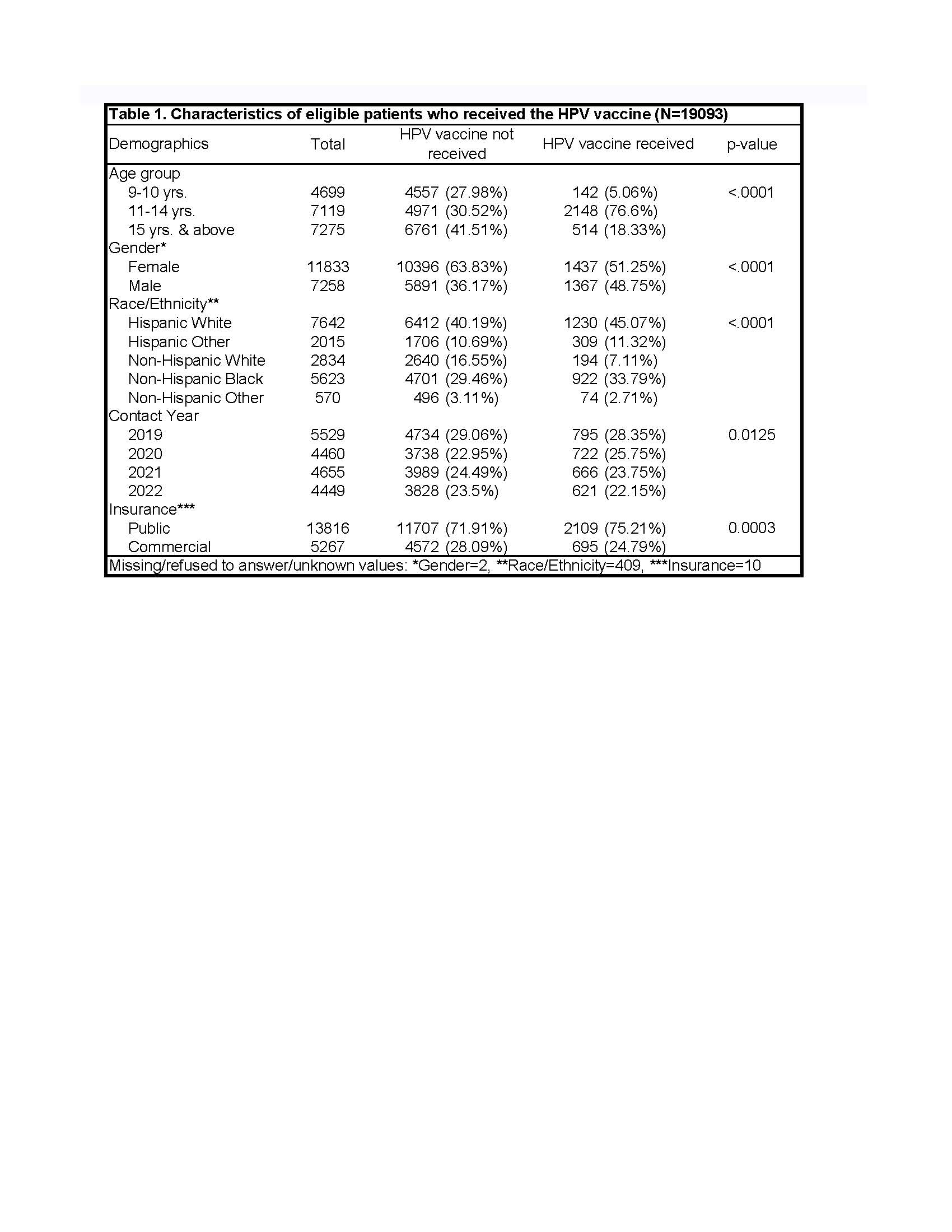
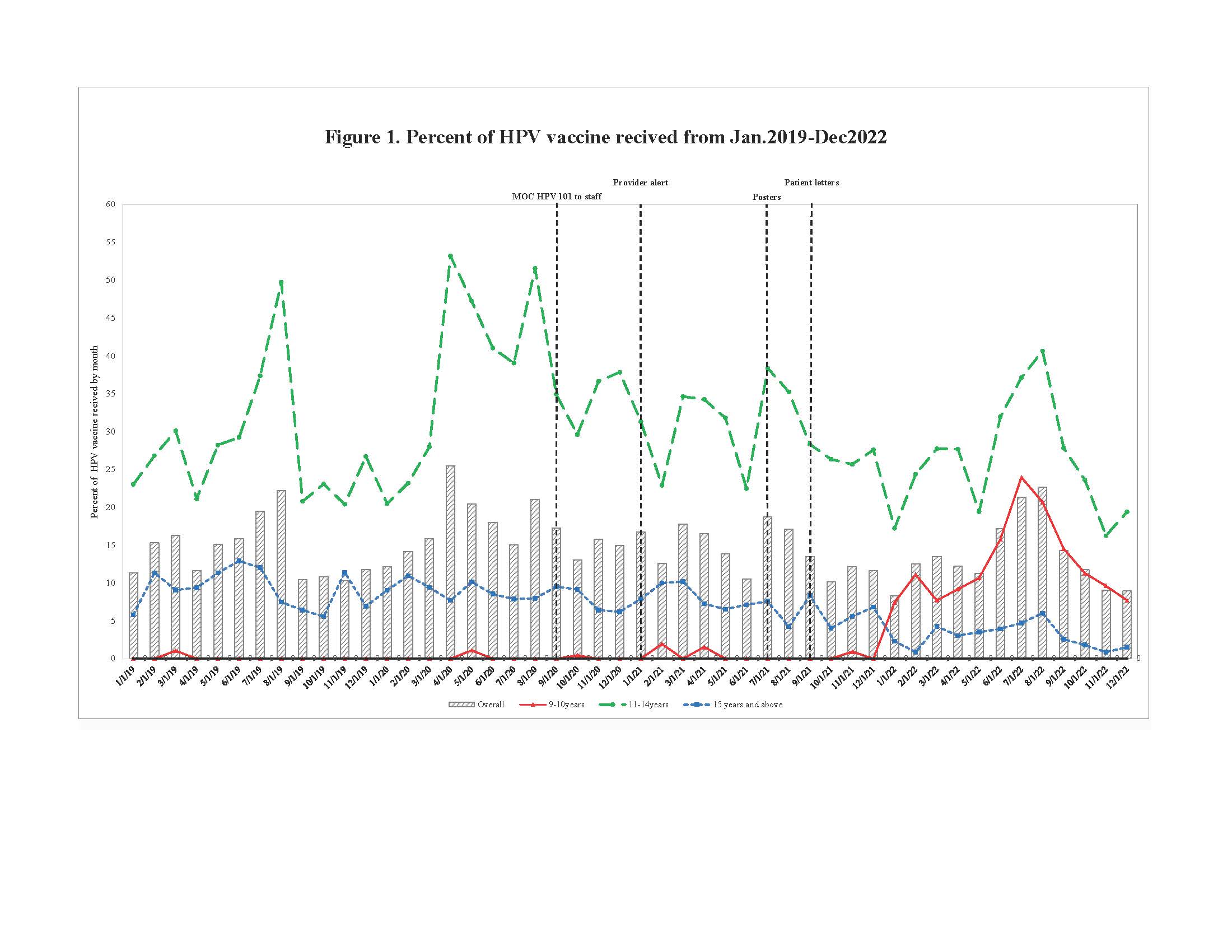
Design/Methods: Structured electronic health record queries identified patients due for an HPV dose and their vaccination status. Mann-Whitney tests, adjusted for observation non-independence, were used to assess differences in demographics and encounter year between those receiving the HPV vaccine and those not. Four quality improvement interventions (staff training, provider alerts, posters, and patient letters) were implemented sequentially, and monthly HPV vaccine uptake was tracked on a run chart.
Results: From 2019-2022 over 4 years, 23,756 encounters were assessed. Of these, 80% (n = 19,093) were eligible for the HPV vaccine, and 15% (n = 2,804) received it during the study. Age-group comparisons revealed vaccination rates of 3% (142 out of 4699) for 9–10-year-olds, 30% (2,148 out of 7,119) for 11–14-year-olds, and 18% (514 out of 7,275) for 15-22-year-olds (p < 0.001). Most vaccine recipients were female (51% vs. 48% male, p < 0.001), Hispanic (55% vs. 7% Non-Hispanic White vs. 35% Non-Hispanic Black, p < 0.001), and had public insurance (75% vs. 25% commercial, p = 0.001). Vaccine uptake per encounter across years was 14% in 2019, 16% in 2020, 14% in 2021, and 14% in 2022 (p = 0.01). Notably, the run chart shows no change in HPV vaccine uptake for 9–10-year-olds, except for a significant increase following patient notification letters.
Conclusion(s): Despite the American Academy of Pediatrics’ universal recommendation for vaccinations at all encounters, our findings reveal an underutilization of HPV vaccinations among 9 to 10-year-old patients. To address this concerning disparity, our findings suggest that quality improvement initiatives should prioritize comprehensive patient education and enhanced communication strategies tailored specifically to boost vaccination rates within this age group.
Funding: K23HD097291, Organon ISP#60445