Neonatology
Session: Neonatal Quality Improvement 3
422 - Quality improvement initiative to increase kangaroo care rates post COVID-19 pandemic at regional perinatal center
Sunday, May 5, 2024
3:30 PM - 6:00 PM ET
Poster Number: 422
Publication Number: 422.2268
Publication Number: 422.2268
- MK
Mary Divya Kasu, MD
Fellow
Jacobs School of Medicine and Biomedical Sciences at the University at Buffalo
Buffalo, New York, United States
Presenting Author(s)
Background: Kangaroo care (KC) or skin-to-skin has been increasingly gaining acceptance and is widely being practiced in the neonatal intensive care unit (NICU). Long-term studies have shown that infants who have undergone consistent KC while in the NICU have increased intellectual quotient (IQ), memory function, and white matter on MRI. However, during the COVID-19 pandemic (2020-2021) the rates of kangaroo care at our regional perinatal center have decreased due to poor family involvement and staffing issues faced by the NICU's across the country.
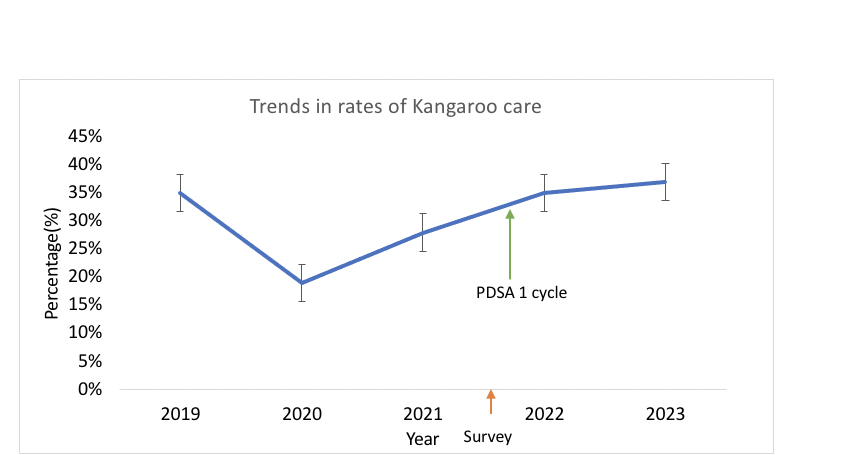
Objective: To understand the barriers and increase the KC rates from 19% during the pandemic to 50%, post-COVID-19 pandemic in our 64 single-bedded regional perinatal center (RPC) level IV NICU
Design/Methods: An 18-question survey was sent out to evaluate the knowledge, attitudes, and barriers to kangaroo care in our unit. Based on the survey results, we initiated online educational modules for the staff. Mannequin-based simulation sessions were done by clinical nurse educators regarding skin-to-skin care for intubated infants. Readiness for kangaroo care was routinely discussed as a part of morning and night rounds at the bedside. A Kangaroo care magnet was placed in the patient’s room when the team decided the infant was ready for skin-to-skin care. Posters and brochures for skin-to-skin care were placed in the family waiting areas and in all the rooms to empower parents towards KC.
Results: A total of 116 responses were received on the survey which included physicians, advanced practice providers, nursing staff, and respiratory therapists. 75% felt comfortable initiating the conversation with families about kangaroo care however only 26% felt comfortable in helping families participate in KC for a 26 weeks gestational age (WGA) compared to 82% for a 32 WGA. Some of the biggest barriers were fear of tube dislodgement (30%), fear of worsening respiratory support in an intubated patient (32%), and nursing refusal (21%)(Figure 1). Based on the responses, we intervened as shown in Figure 2. Our pre-pandemic KC rates were 35% which plummeted to an all-time low at 19% during the COVID-19 pandemic but after our interventions and the first PDSA cycle improved to 28% in 2022 and 38% in 2023. (p=0.003)(figure 3)
Conclusion(s): The COVID-19 pandemic led to changes in policies in health care across the world. Though we saw an improvement after our first PDSA cycle, this is an ongoing project and for the next PDSA cycle, our goal is to improve the KC rate further to 50% in the next quarter.
.png)
.png)
