Neonatology
Session: Neonatal Quality Improvement 3
419 - Increasing Early Mobility in a Level IV NICU: Adaptation and Implementation of PICU Up! Bundle in the NICU
Sunday, May 5, 2024
3:30 PM - 6:00 PM ET
Poster Number: 419
Publication Number: 419.2277
Publication Number: 419.2277
.jpg)
Brooke A. Krbec, DO, MS
Neonatologist
Floating Hospital for Children at Tufts Medical Center
West Roxbury, Massachusetts, United States
Presenting Author(s)
Background: The medical complexity and acuity of critically ill neonates often leads to inadequate focus or exclusion from developmental care therapies. Structured interdisciplinary approaches to promote early mobility can improve outcomes. PICU Up!TM is a novel multidisciplinary bundle of cares developed to increase early mobility in pediatric intensive care unit (ICU) patients.
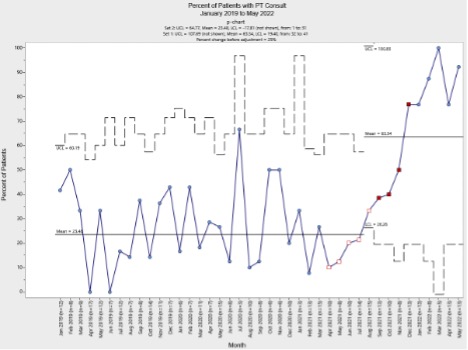
Objective: Our goal was to implement an adapted PICU Up!TM Guideline to establish a consistent early mobility strategy and increase developmental therapy use in the Boston Children’s Hospital NICU for surgical infants at ≥34 weeks post-menstrual age (PMA). Our specific aim was to increase the percent of eligible surgical patients with physical therapy (PT) consults from a baseline of 27% to greater than 50% over a 6-month pilot period.
Design/Methods: Our multidisciplinary team modified the PICU Up!TM Guideline for neonatal patients after identifying change ideas via a needs assessment survey distributed to NICU staff. An introductory plan was developed, involving personalized staff education, two shadow pilots ensuring infants admitted met guideline criteria, and addition of PICU Up!TM level and mobility goal parameters to EMR flowsheets and nursing handoff sheets to enhance compliance with this new metric. Interventions were tested using a quality improvement framework and Plan Do Study Act cycles included addition of a prompt on daily rounds discussion sheet, structured staff education, and optimization of documentation. Data was collected each week from November 2021 to May 2022. SPC charts generated using Chartrunner software tracked key project measures over time. Significant changes, such as shifts in the mean during the project period were noted. P-charts displayed the main outcome measures, while X-bar S-charts depicted the process measure.
Results: A significant increase was demonstrated in the number of surgical patients with PT consultations from a baseline of 23.5% to 63.5% with special cause variation on SPC analysis and the final 6 months of analysis all greater than 80%. SPC chart analysis showed a reduction in variability after project start with special cause variation and a trend towards significant decrease in both NICU length of stay and mean ventilator days. The rate of pressure injuries remained low and stable. Balancing measures of unplanned extubations and fractures have had no change.
Conclusion(s): Together, successful institution of a standardized early mobility guideline increased focus on increasing developmental cares and increased use of physical therapy consultations in post-operative NICU patients.