Nephrology
Session: Nephrology 1
8 - Microbial Etiology and Antibiotic Resistance Patterns of Urinary Tract Pathogens in Hospitalized Children: A Single-Center Experience
Saturday, May 4, 2024
3:30 PM - 6:00 PM ET
Poster Number: 8
Publication Number: 8.1089
Publication Number: 8.1089
- MT
Michelle H. Talukder, M.D (she/her/hers)
Resident
Children's Hospital of Michigan
Detroit, Michigan, United States
Presenting Author(s)
Background: Urinary tract infections (UTIs) are common in children. Early diagnosis and prompt treatment are crucial to avoid complications. However, providing appropriate empirical antibiotic treatment is challenging for any clinician while waiting for 48 hours for susceptibility results, considering the rise in urinary pathogens resistant to commonly used antibiotics, especially with the emergence of extended-spectrum beta-lactamase (ESBL)-producing organisms.
Objective: Our study aims to investigate the local resistance patterns of uropathogens causing acute UTI in hospitalized children at Children's Hospital of Michigan during a 3-year period and to provide guidance for the preferred choice of empirical antibiotic treatment at the time of diagnosis.
Design/Methods: We conducted a retrospective study that included children aged >1 month and < 18 years admitted for acute UTI between April 1, 2020, and March 31, 2023. UTI defined as positive urine culture with a single microorganism of >= 100,000 colony-forming units (CFU)/mL. Patients with inappropriate method of urine collection, on intermitted catheterization and immunocompromised were excluded. We used SAS (version 9.4) to perform statistical analysis.
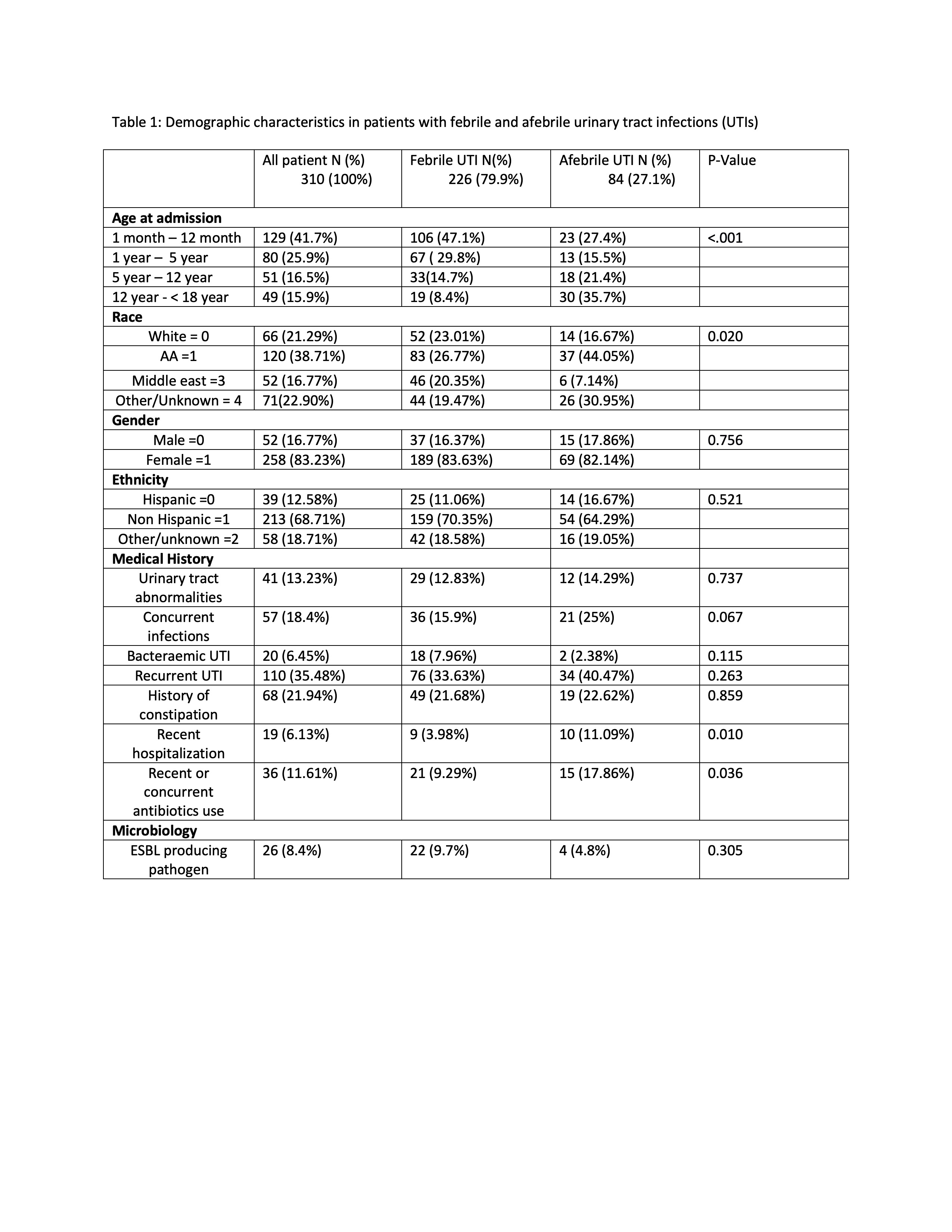
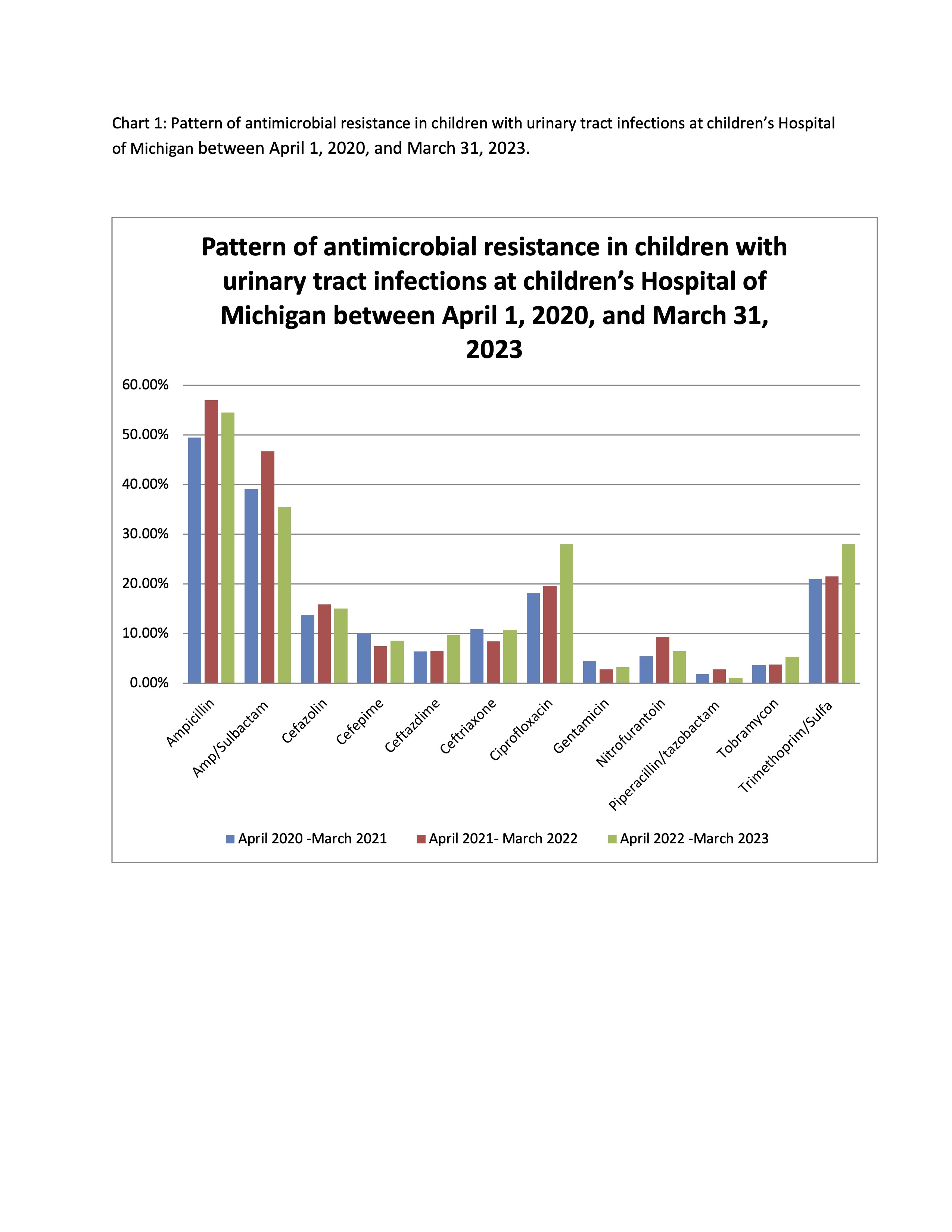
Results: Data from 310 children were analyzed, with 83% being female. The majority of patients (42%) were under one year of age, and 87% were generally healthy without underlying urological abnormalities. A notable portion had a previous history of UTI (35%) or constipation (22%) (table 1). Afebrile UTIs were significantly associated with recent hospitalization (p=0.010) and antibiotic use within the last 30 days before UTI onset (p=0.036). The predominant causative organism was Escherichia coli (E.Coli), identified in 83% of patients, followed by Klebsiella pneumonia (7%), with 24 out of 257 (9%) being E.coli ESBL-producing organisms. All microorganisms exhibited the highest resistance to Ampicillin (54%), followed by Amp/Sulbactam (41%). Trimethoprim/Sulfamethoxazole resistance slightly increased to (28%) during April 2022-March 2023 from (22%) the previous two years. Cephalosporin antibiotic resistance was highest against Cefazolin (a first-generation cephalosporin) at (15%). Aminoglycosides demonstrated low resistance rates among all cultured uropathogens (4%), and carbapenem resistance was lowest at (0.3%).
Conclusion(s): E. coli is the predominant uropathogen causing acute UTI during childhood. Our data suggest an increasing resistant trend to Ampicillin and Trimethoprim/Sulfamethoxazole. Cephalosporins may be the most appropriate choice of antibiotic as empirical treatment for acute UTI in our community.