Nephrology
Session: Nephrology 4
17 - Association Between Blood Pressure with Left Ventricular Systolic Function in the Chronic Kidney Disease in Children Study
Sunday, May 5, 2024
3:30 PM - 6:00 PM ET
Poster Number: 17
Publication Number: 17.2282
Publication Number: 17.2282

Alex Kula, MD, MHS
Assistant Professor of Pediatric Nephrology
Ann & Robert H. Lurie Children's Hospital of Chicago
Chicago, Illinois, United States
Presenting Author(s)
Background: Youth with chronic kidney disease (CKD) often demonstrate reduced left ventricular systolic global longitudinal strain (LV GLS) on echocardiography. Hypertension is a risk factor for relatively worsened LV GLS in pediatric CKD. While most studies demonstrate youth with CKD have relatively lower LV GLS, it is unclear what proportion demonstrate abnormal LV GLS using the adult consensus definition of < 16%.
Objective: The objective of this study was to test the association between elevated blood pressure (BP) with abnormal LV GLS in youth with mild to moderate CKD.
Design/Methods: This was an ancillary study of the chronic kidney disease in children (CKiD) study. Echocardiograms were reanalyzed by a pediatric cardiologist to generate LV GLS values. The primary outcome was an LV GLS < 16%. The primary exposure was casual BP. Generalized estimating equations (GEE) were used to account for within-person correlation and estimate robust standard errors for 95% confidence intervals (95% CI). Covariates in adjusted models included: age, sex, race, estimated glomerular filtration rate (eGFR), urine protein (UPC), hemoglobin, LVH, use of ace-inhibitors. Casual BP parameters were defined using 2017 AAP guideline definitions. Secondary analyses using ambulatory BP monitoring (ABPM) was performed in participants with available data (n=582).
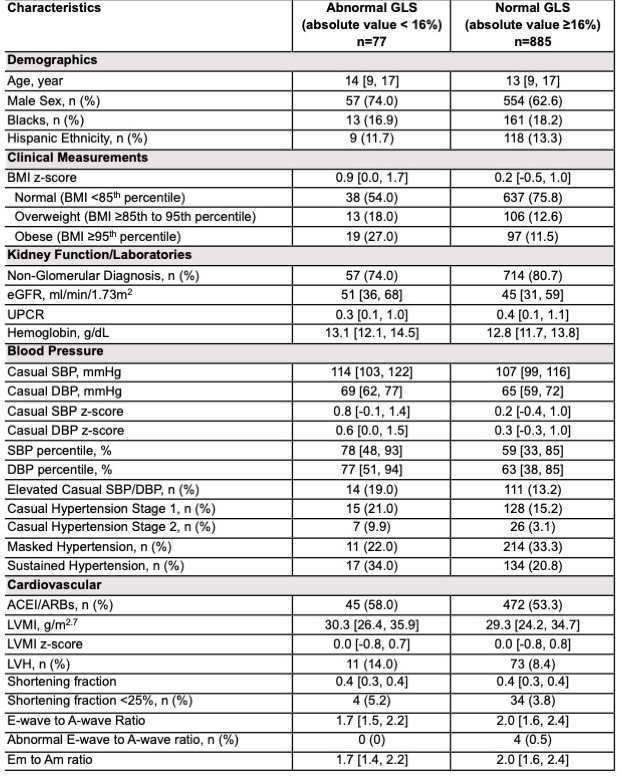
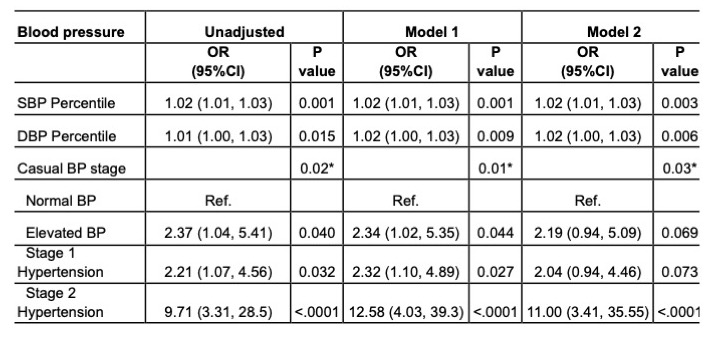
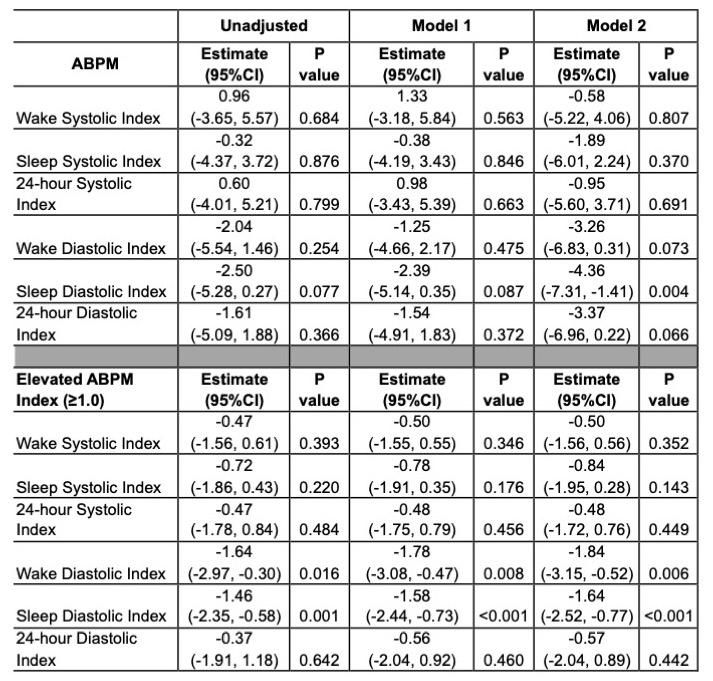
Results: LV GLS was measured in 962 person-visits. A total of 77 (8%) had an LV GLS < 16%. Baseline characteristics between those with a normal and abnormal LV GLS are included in Table 1. In fully adjusted models, higher eGFR was associated with increased odds for abnormal LV GLS, but age, race, sex, UPC, and hemoglobin were not significantly associated. Several casual BP parameters, including SBP and DBP percentile and the presence of stage 2 hypertension were significantly associated with abnormal LV GLS (Table 2). The only ABPM parameter associated with abnormal LV GLS was sleep diastolic index (p=0.004, Table 3).
Conclusion(s): In total, 8% of youth with mild to moderate CKD enrolled in the CKiD study had abnormal systolic function. Elevated diastolic blood pressure was an important determinant of abnormal LV GLS. Future studies should focus on elucidating the link between diastolic hypertension and abnormal LV GLS.