Neonatology
Session: Neonatal Follow-up 3
538 - Medical Needs of Very Low Birth Weight Preterm Infants Following Hospital Discharge: Home Oxygen Therapy and Outpatient Resource Utilization
Monday, May 6, 2024
9:30 AM - 11:30 AM ET
Poster Number: 538
Publication Number: 538.2733
Publication Number: 538.2733
.jpg)
Jui-Hsing Chang, Neonatologist
Attending neonatologist
MacKay Children's Hospital
Taipei, Taipei, Taiwan (Republic of China)
Presenting Author(s)
Background: Premature infants with a birth weight less than 1,500 grams (very low birth weight, VLBW) accounted for nearly 1% of all neonates in Taiwan. Discharge isn't the end of their health problems.
Objective: We used the data from Taiwan Premature Infant Follow-up Network (TPFN) database to explore the conditions of these children at discharge, medical assistive devices at home, and interdisciplinary medical needs at two years of age.
Design/Methods: This study was based on neonatal, and 2-year-old follow up data of VLBW infants registered in TPFN between 2011-2017. Basic information, survival and conditions during hospitalization were recorded. Medical needs at discharge, outcomes at the corrected age of 24 months, involvement in out-patient health care services and referrals were investigated. We also explored the incidence and predicting factors of home oxygen therapy (HOT) in infants with chronic lung disease (CLD). In infants of CLD, 2-year-old outcomes were compared between patients with and without HOT.
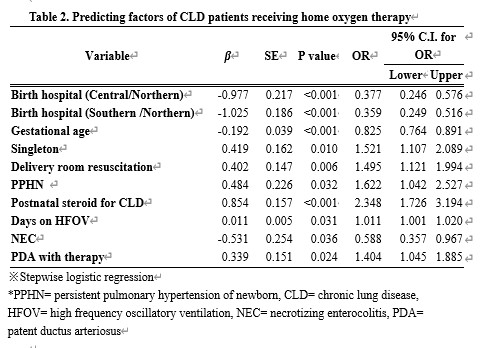
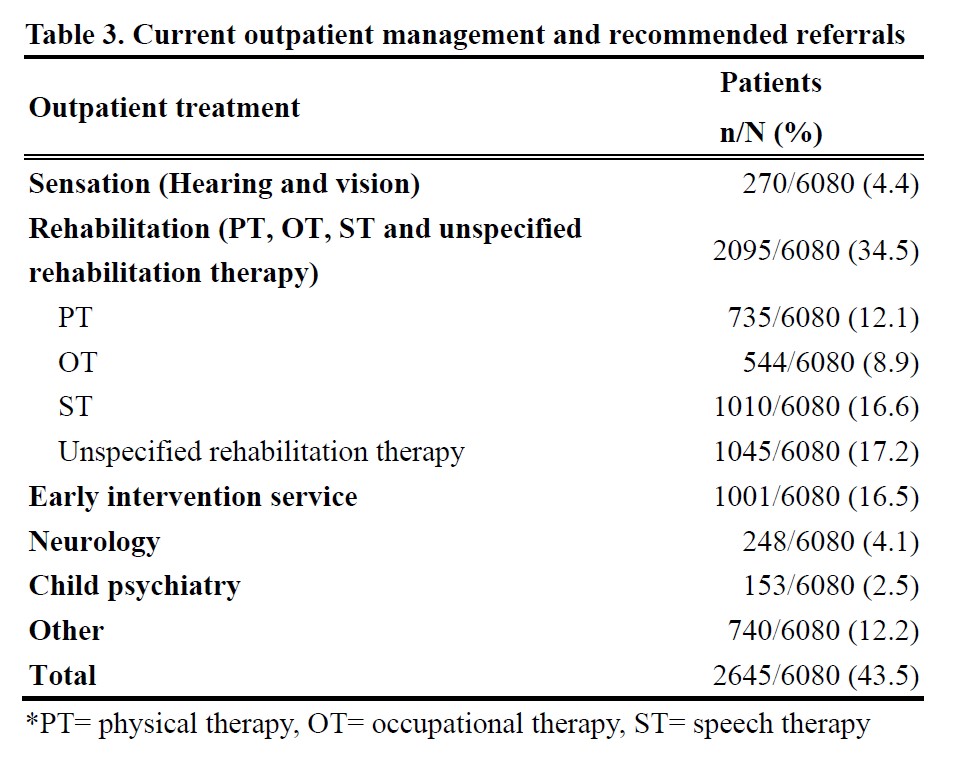
Results: A total of 9,243 VLBW preterm neonates were enrolled, 140 of whom were excluded for congenital anomalies, and 7,949 survived to discharge. 40 children died between discharge and two years old, and 6150 people came back for follow-up evaluation. At discharge, 10.2% of patients received HOT. Home monitoring devices were used in 6.5% of patients. CLD was diagnosed in 35.6% of patients surviving to 36 weeks of postmenstrual age. 26.6% of CLD patients using HOT. Birth hospital, gestational ages, singleton, delivery room resuscitation, and some severe morbidities during hospitalization were significantly related to HOT. Regarding current treatment and recommended referrals at 2 years of corrected age, rehabilitation treatment accounted for the most (34.5%), followed by early intervention system services (16.5%), visual or hearing assessment and treatment (4.4%), neurologic follow up (4.1%), and mental health assessment and treatment (2.5%). At 2 years of corrected age, more children of CLD with HOT had poor growth compared to CLD patients without HOT. HOT group had lower language and motor developmental scores.
Conclusion(s): The use of medical assistive devices and out-patient health services are substantial in VLBW preterm infants after hospital discharge. At 2 years of age, the most needed out-patient health service or referral item is rehabilitation treatment. CLD patients with HOT are prone to having growth and developmental delay. Providing sufficient rehabilitation-related medical treatment after discharge and the adequacy of early intervention and education systems are worthy of attention.
.jpg)