General Pediatrics
Session: General Pediatrics 2
248 - N-NIP it in the bud: Nursing-directed Nudges to Increase Preventive visits for children who are overdue for well care
Friday, May 3, 2024
5:15 PM - 7:15 PM ET
Poster Number: 248
Publication Number: 248.5
Publication Number: 248.5

Katie E. McPeak, MD (she/her/hers)
Associate professor of Clinical Pediatrics
Perelman School of Medicine at the University of Pennsylvania
Narberth, Pennsylvania, United States
Presenting Author(s)
Background: Acute visits are a potential missed opportunity to deliver holistic preventive care. In our analysis, 80% of patients who had not been seen for timely preventive care had been seen at least once within the 12-month lookback period for an acute visit within their medical home. These visits were typically for low acuity conditions, such as constipation, eczema, or upper respiratory infections. Our team concluded that a successful intervention to improve preventive care could reside at the point of contact when a family reaches out for an acute concern.
Objective: Can a nursing-directed nudge increase preventive care for children who are overdue?
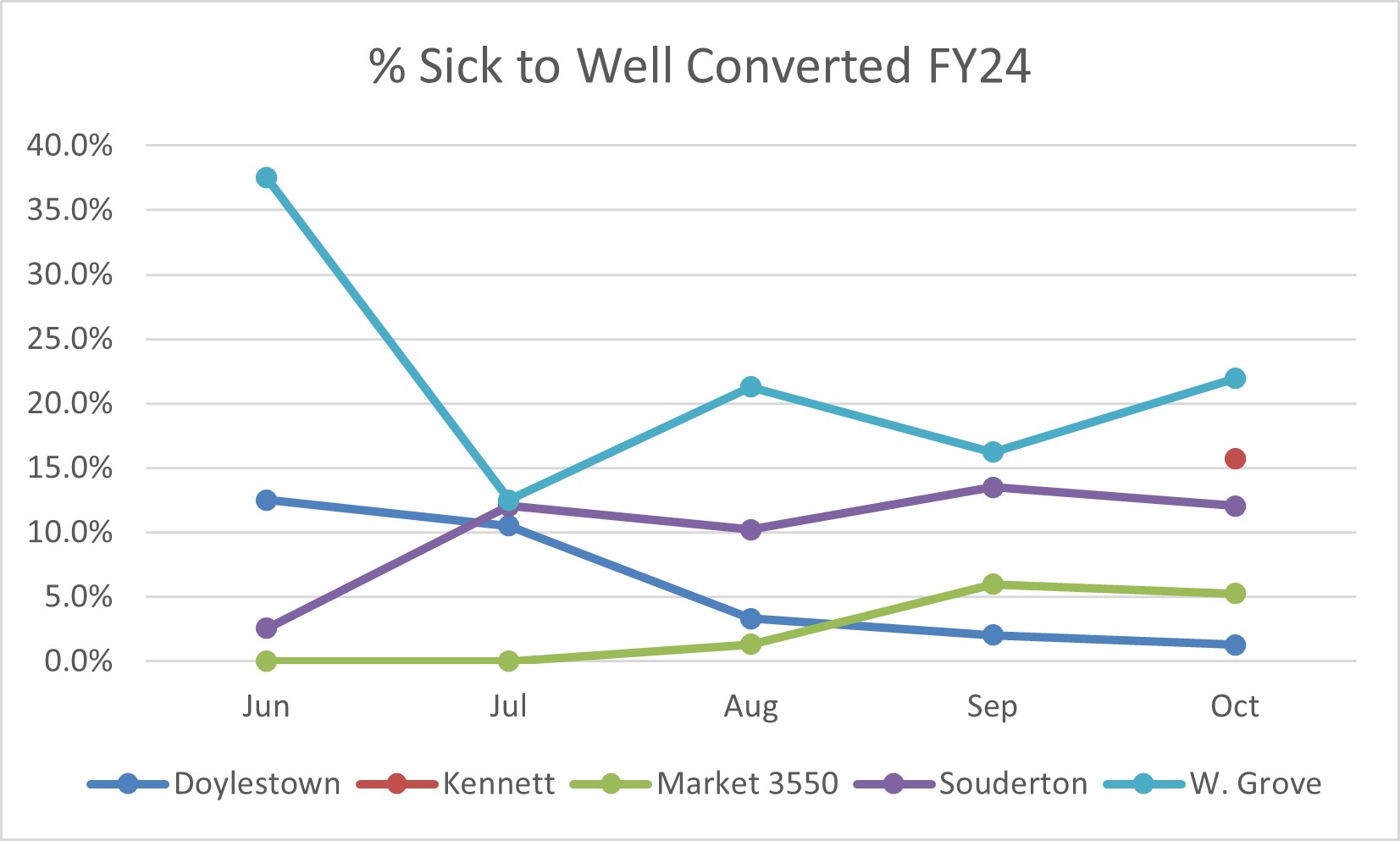
Design/Methods: Using planned sequential interventions and innovation ecosystem design, our team designed and implemented an alert that would inform nurses and office staff on sick triage calls if a child was overdue for preventive care. The alert was built with specific criteria such as patient age and appointment date logic that appears in the nursing telephone encounter template workflow. 4 network sites initially volunteered in summer 2023 to test the intervention. Nurses were given choices of appointment outcome options from which to choose if the alert fired. A 5th site was selected in September 2023. The 5th site cares for a more rural population with over 15% of the population preferring Spanish for spoken communication. Collectively, these sites care for over 20,000 children and represent a mix of urban/rural/suburban with varying insurance coverage. The pilot practices combined care for approximately 15% of our total primary care network population.
Results: From 6/15/23- 10/16/23, the alert fired for 1490 encounters across the 5 pilot sites. 141 (9.4%) of eligible encounters were converted to well visits whereby the clinician could address both the acute concern and conduct a preventive visit on the same encounter. Well visit types were used by the RN to signal correct visit type and assign previsit screeners (i.e., developmental screening). Though there was initial fear of overload and stress on health care teams, only 47 of the eligible triage calls (3.15%) were not accommodated due to “office unable to accommodate.”
Conclusion(s): Taken in concert with other measures, nudging nurses to convert a potential sick visit to a well visit can be a successful, family-centered intervention to improve attainment of preventive care. To improve health equity, this intervention should be preferentially considered in less resourced, higher poverty communities, where access to primary care is historically suboptimal and families face more barriers to care.
.jpg)