Medical Education
Session: Medical Education 6
425 - Implementing and Evaluating a Resident Curriculum on the Health Effects of Climate Change
Saturday, May 4, 2024
3:30 PM - 6:00 PM ET
Poster Number: 425
Publication Number: 425.1678
Publication Number: 425.1678

Charles E. Moon, III, MD (he/him/his)
Chief Resident
The Children's Hospital at Montefiore
Bronx, New York, United States
Presenting Author(s)
Background: The American Academy of Pediatrics and other healthcare organizations have policy statements that support integrating the health effects of climate change (CC) into medical education as an essential component of preparing trainees for this evolving environmental and public health emergency. However, implementation of this topic into graduate medical education and residency program curricula remains in its infancy, lacking standardization or evaluation.
Objective: To assess the effects a CC educational session on resident understanding and confidence regarding: (1) the effects of CC on human health; (2) appropriate anticipatory guidance and community resources to provide to patients and families about the health effects of CC; (3) utilizing anticipatory guidance in future medical visits with patients and families. To assess differences between small group and lecture-based learning formats for the sessions.
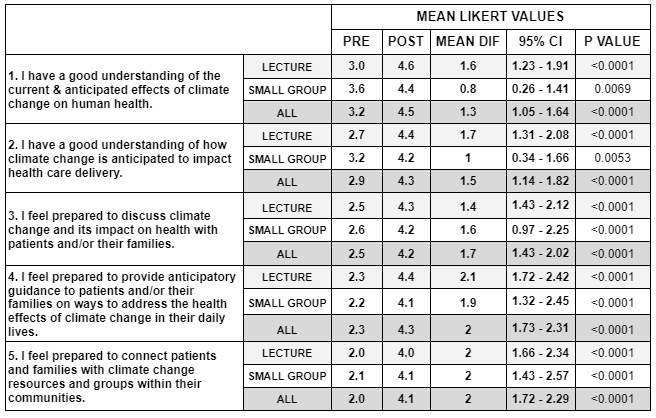
Design/Methods: A novel CC educational session was created in a large academic health center in the Bronx and integrated into Pediatrics and Family Medicine residency programs’ educational programming. The session used learning objectives linked to Accreditation Council for Graduate Medical Education competencies and emphasized local evidence-based health guidance easily integrated into clinical practice. Residents participated in 1 of 3 separate 90 minute small group or lecture-based sessions. A pre- and post-session 5 question Likert-scale survey was created to assess resident understanding of CC health effects and confidence in providing CC-informed healthcare delivery. Pre and post-session responses were compared using paired t-tests. Differences in learning between small group or lecture-based formats was assessed with a pooled t-test.
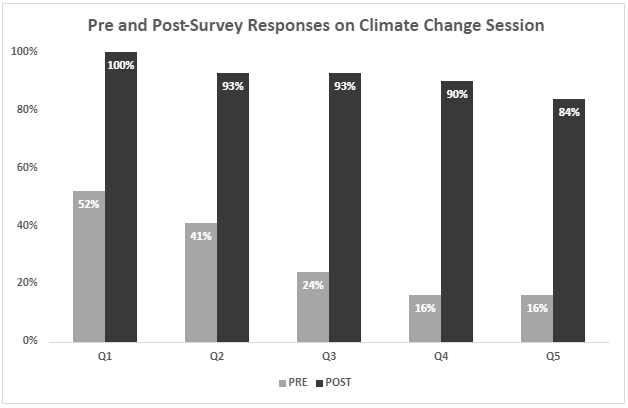
Results: 58 resident participants completed a 5 question pre- and post-session survey (18 small group, 40 lecture-based format). Residents’ understanding and confidence in engaging with patients and families on the health effects of CC after the curricular session improved (Figure 1) and was statistically significant (Table 1). No difference was found between learning formats (p=0.161).
Conclusion(s): A novel CC curriculum was effective at increasing the understanding of the health effects of CC and confidence utilizing anticipatory guidance and resources on CC with patients among pediatric and family medicine residents. It may serve as a framework for implementation of this topic in other residency program curricula. Further study to investigate the most effective teaching modalities and timing in resident training is needed to further refine CC curriculum.