Neonatology
Session: Neonatal Quality Improvement 2
406 - Reducing unnecessary morphine exposure in mechanically ventilated neonates: a quality improvement program
Sunday, May 5, 2024
3:30 PM - 6:00 PM ET
Poster Number: 406
Publication Number: 406.1705
Publication Number: 406.1705
Huayan Zhang, MD
Neonatologist
Children's Hospital of Philadelphia/Guangzhou Women and Children's Medical Center
Philadelphia, Pennsylvania, United States
Presenting Author(s)
Background: The importance of sedation and pain management in mechanically ventilated neonates has been accepted in the Chinese NICUs in the recent years. However, overzealous use of narcotics can be harmful. We have found that 90% (range 81-100%) of the neonates undergoing mechanical ventilation in our NICU were receiving continuous morphine infusions.
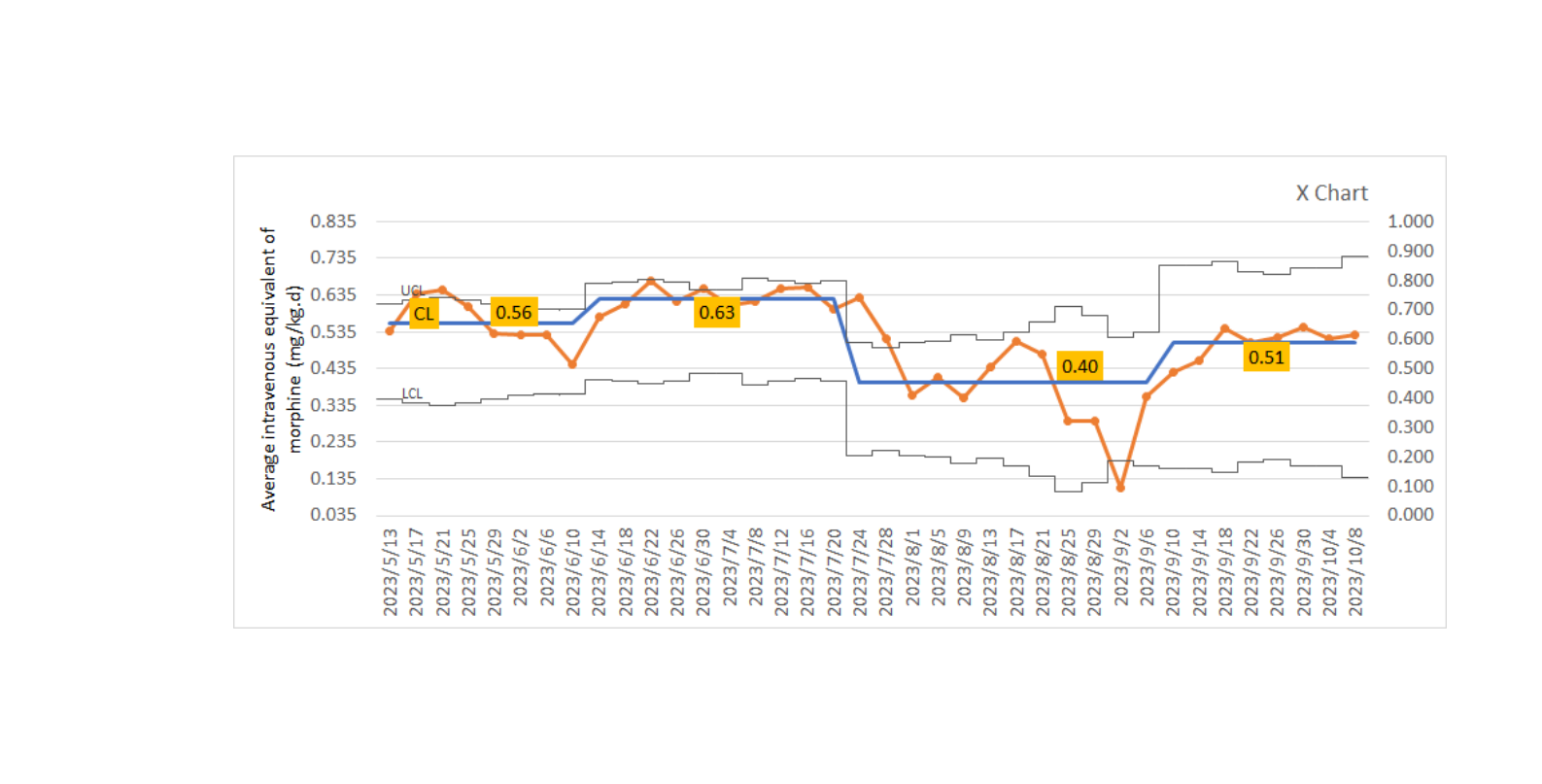
Objective: This single center quality improvement (QI) initiative aimed at reducing continuous morphine exposure in mechanically ventilated infants in our NICU by 20% in 5 months from May to September 2023.
Design/Methods: A multidisciplinary QI team including neonatologists, neonatal nurses, anesthesiologist and pharmacist was assembled. After literature review, multiple team discussions, benchmarking and effect analysis, a key driver diagram was developed (Fig.1) and the key interventions was decided to center around implementing a standardized evidence-based sedation and analgesia protocol. Interventions to support the implementation of this protocol included proper use of neonatal pain assessment scales (CRIES) and State Behavior Scales (SBS) assessment tools, employing nonpharmacological treatment measures, placement of warning signs, setting up screensavers on all work computers, routine discussions of pain management during medical team rounds, reporting the number of continuous morphine use in ventilated patients during daily morning sign-outs, regular data feedback, and a series of training and education for NICU providers. The primary and secondary outcome measures were the rate of continuous morphine exposure and the average daily dose of intravenous (IV) equivalent morphine. Average daily dose of midazolam and incidence of unplanned extubations were set as balancing measures. Data was collected and analyzed using run charts and control charts.
Results: The rate of continuous morphine exposure in mechanically ventilated neonates decreased by 46% from 90% to 49% with the average daily dose of IV equivalent morphine decreased from 0.56mg/kg to 0.51mg/kg (Figures 2,3). After education for SBS implementation and proper CRIES were carried out, compliance of SBS and CRIES increased from 86% and 83% to 94% and 88%, respectively, both with accuracy exceeding 90%. The average daily use of midazolam remained unchanged at 0.23mg/kg. Only one unplanned extubation occurred during this QI period.
Conclusion(s): QI measures focusing on standardized sedation and analgesia protocol for mechanically ventilated patients in NICU can reduce unnecessary continuous morphine exposure.
.png)
.png)
