Neonatology
Session: Neo-Perinatal Health Care Delivery 4: Epidemiology/Health Services Research
277 - Social Determinants of Health and Oxygen Use in Preterm Infants with Bronchopulmonary Dysplasia
Sunday, May 5, 2024
3:30 PM - 6:00 PM ET
Poster Number: 277
Publication Number: 277.1706
Publication Number: 277.1706
.jpg)
Bridget Dillon, DO, MS (she/her/hers)
Neonatal-Perinatal Medicine Fellow
Children's Hospital of Michigan
Dearborn, Michigan, United States
Presenting Author(s)
Background: Social disparities can negatively impact post-discharge outcomes in preterm infants with bronchopulmonary dysplasia (BPD). The Child opportunity index (COI) is a publically available indicator of neighborhood inequities and quality of resources in the communities.
Objective: The aim of our study is to examine the association between COI scores and duration of home oxygen use in preterm infants with BPD discharged on home oxygen therapy.
Design/Methods: After obtaining IRB approval, a retrospective study of preterm infants with birth weight < 1,250 grams, discharged on home oxygen from NICU and followed up outpatient in the BPD clinic from January 2010 to January 2022 was conducted. Data were gathered on maternal and infant demographics, clinical data during hospital stay, ZIP code, insurance, number of people living in the house, cigarette smoking, and duration of home oxygen, missed clinic appointments, readmissions and emergency room visits. COI scores were obtained based on zip codes and neighborhoods stratified into very low, low, moderate, high or very high opportunity levels. Our primary outcome is time to wean off home oxygen and secondary outcomes are emergency room visits, readmissions and missed BPD clinic appointments. Demographic characteristics of our cohort were described using descriptive statistics as appropriate. ANCOVA was used to analyze association of COI scores and duration of home oxygen after adjusting for gestational age (GA), length of stay and days of invasive mechanical ventilation (MV).
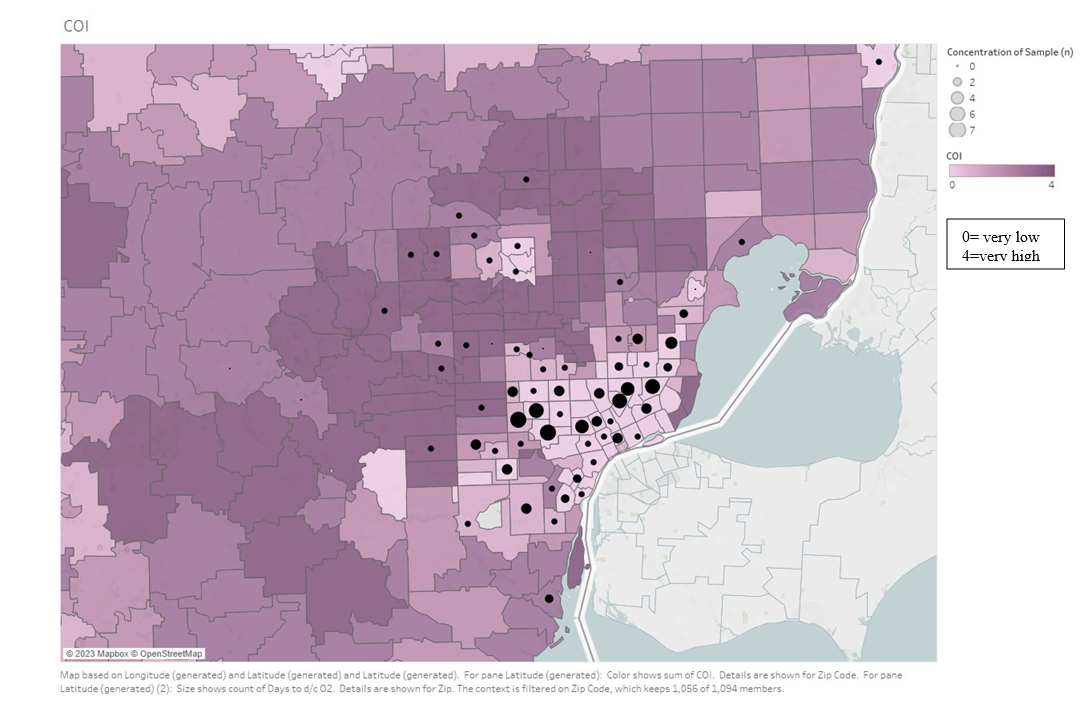
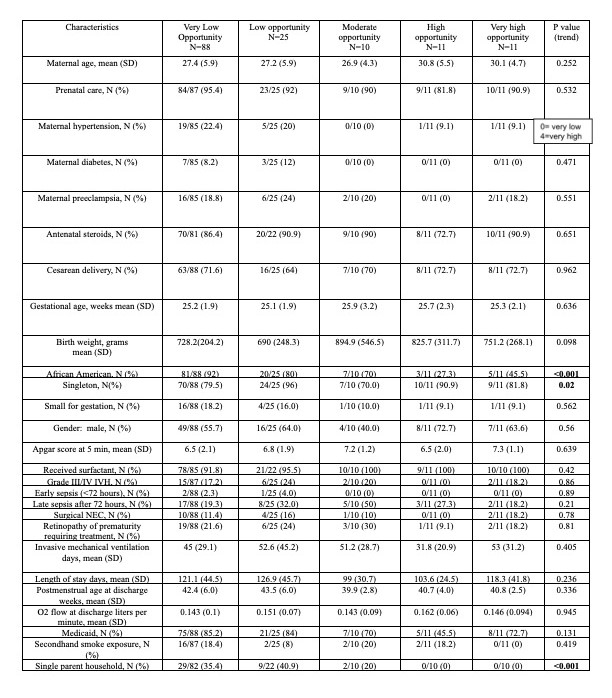
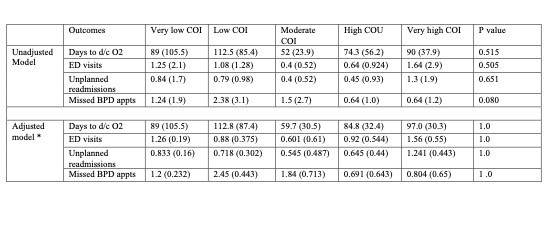
Results: Our cohort had 146 infants; mean (SD) gestational age was 25.3 (2.1) weeks, mean (SD) birth weight was 755 (271) grams, 116 (80%) were black and 84 (57.5%) were males. The highest proportion of infants (60%) resided in the very low COI areas. Figure 1 shows the distribution of infants based on COI levels. There was a statistically significant difference in the proportion of black infants and single parent household in the very low COI areas compared to high and very high COI areas (Table 1). Mean (SD) for duration of home oxygen was 89.5 (92) days for the entire cohort- 89 (105) days for the very low COI and 90 (37.9) days for the very high COI areas. On ANCOVA after adjusting for GA, length of stay and MV days no statistical difference was noted in the duration of oxygen use or any secondary outcome (Table 2). We noted a trend of increasing number of oxygen days with lower COI levels.
Conclusion(s): The duration of home oxygen use did not vary with COI levels. This could possibly be the result of disproportionate distribution of our sample.