Medical Education
Session: Medical Education 5
403 - Addressing Challenges to Resident High-Value Care Practice at an Academic Children’s Hospital: A Curriculum for Senior Pediatric Residents
Saturday, May 4, 2024
3:30 PM - 6:00 PM ET
Poster Number: 403
Publication Number: 403.1663
Publication Number: 403.1663
- PS
Patrick Snyder, MD, MBA (he/him/his)
Critical Care Medicine Fellow
Children's Hospital Colorado
Denver, Colorado, United States
Presenting Author(s)
Background: United States healthcare costs are increasing at an unsustainable rate. Physicians contribute to overdiagnosis and overtreatment. Residents need to learn value-based care. ACGME requires residents to incorporate considerations of cost-awareness in patient care. Yet, providing high-value care (HVC) can be challenging for residents working in environments with high acuity services, consultants, and lack of cost transparency.
Objective: To develop, implement, and evaluate a curriculum on high-value care for senior (PGY-2-4) pediatric and medicine-pediatric residents.
Design/Methods: We designed a new HVC Academic Half Day (3.5-hour block conference) for a large pediatric residency program (n=94 residents). The curriculum, taught in March 2023, consisted of 4 learning activities: an overview lecture of HVC principles; a small group case-based discussion (child with orbital cellulitis) working with consultants on a hospital medicine service; a small group case-based discussion utilizing an interactive cost dashboard to manage a child hospitalized with bronchiolitis in the pediatric intensive care unit (PICU); and a case competition focused on a cost-conscious diagnostic evaluation.
Evaluation consisted of an electronic retrospective post-then-pre survey which residents accessed via a QR code. Findings were analyzed with descriptive statistics and basic qualitative analysis of open-ended questions.
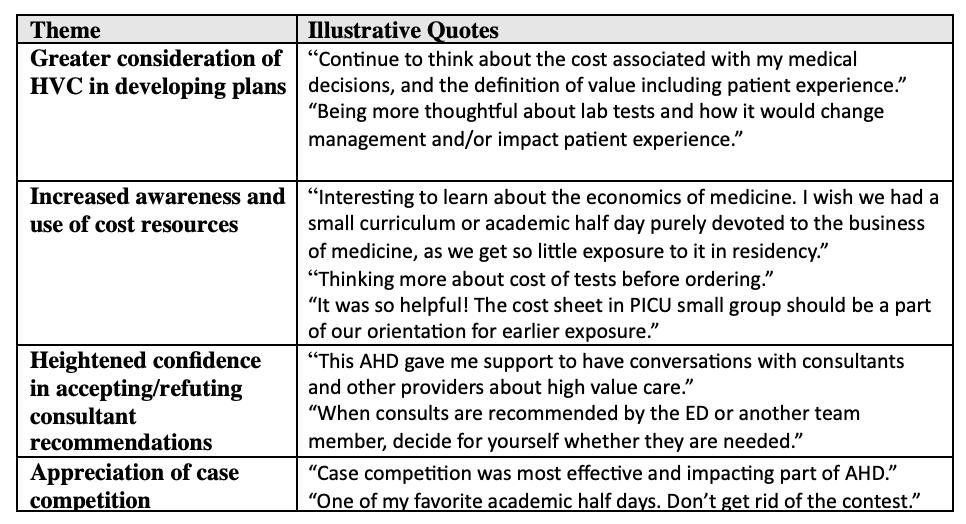
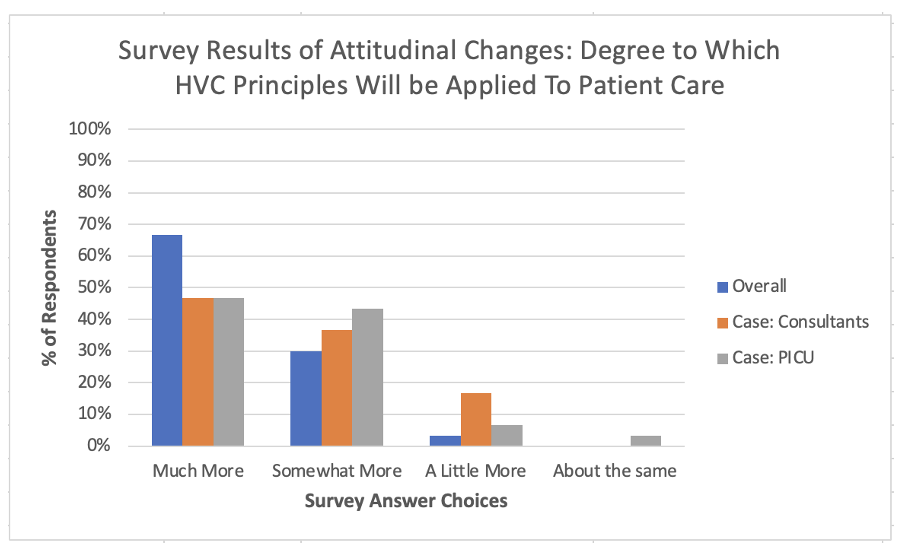
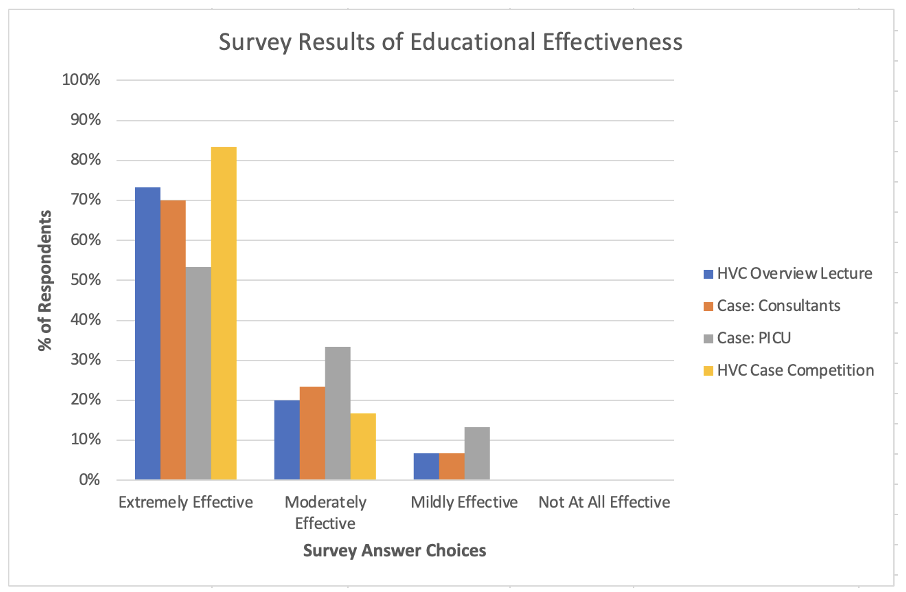
Results: Forty-five pediatric residents were scheduled to complete the curriculum. Survey results (response rate 67%) revealed 97% of residents were “much/somewhat more” likely to incorporate considerations of cost-awareness after participating in the curriculum. Respondents were also “much/somewhat more” likely to apply HVC principles with consultants (84%) and to patients in the PICU (90%) (Figure 1). Nearly all found the curricular components to be “extremely/moderately effective” (Figure 2). Themes from qualitative analysis included: greater consideration of HVC in developing plans, increased awareness and use of cost resources, heightened confidence in managing consultant recommendations, and appreciation for the case competition due to curriculum participation (Table 1).
Conclusion(s): We successfully developed, implemented, and preliminarily evaluated an HVC curriculum uniquely focused on low-value contexts, working with consultants, the PICU environment, and lack of cost transparency. Results highlight perceived planned changes in behavior to incorporate HVC principles. Next steps include evaluating the impact of this curriculum on senior resident clinical practice and designing a curriculum for interns.