Medical Education
Session: Medical Education 4
394 - Innovative Disability Curriculum Integration for Procedural Clinical Skills: Enhancing Competence and Confidence Among Third Year Medical Students
Saturday, May 4, 2024
3:30 PM - 6:00 PM ET
Poster Number: 394
Publication Number: 394.1658
Publication Number: 394.1658
- CM
Christine Murphy, MD (she/her/hers)
Division Chief Pediatric Developmental Disabilities
Texas Scottish Rite Hospital for Children
Dallas, Texas, United States
Presenting Author(s)
Background: Accrediting bodies in medical education, at both graduate and undergraduate levels, historically overlook explicit competencies for procedural clinical skills in disability education. Even within specialized fields like Pediatrics and Med/Peds, a comprehensive literature review exposes a notable deficiency in explicit training. Remarkably, this persists despite approximately 27% of American adults experiencing at least one disability (source: CDC). Roughly 28 in 100,000 U.S. adults require g-tube or trach use (source: PMC), and lack of physician training has been cited as a key driver of discrimination for children with medical complexity (source: Pediatrics).
Most medical students are likely to care for patients with devices like gastrostomy tubes and tracheostomies, yet there is no standardized formal training or competency assessment for these procedures in medical schools or residencies. Physicians often serve as the final recourse in case of device failure or complications, emphasizing the need to address this training gap.
Objective: This educational innovation aimed to formalize the educational curriculum and introduce formative assessments for gastrostomy and tracheostomy care and changes, producing proficient physicians who can comfortably care for patients with these devices, improving healthcare access.
Design/Methods: Curricular mapping revealed limited skills teaching for all students, despite clerkships beginning in the third year. Introduction to Clerkships course students were chosen for training just prior to clinical rotations.
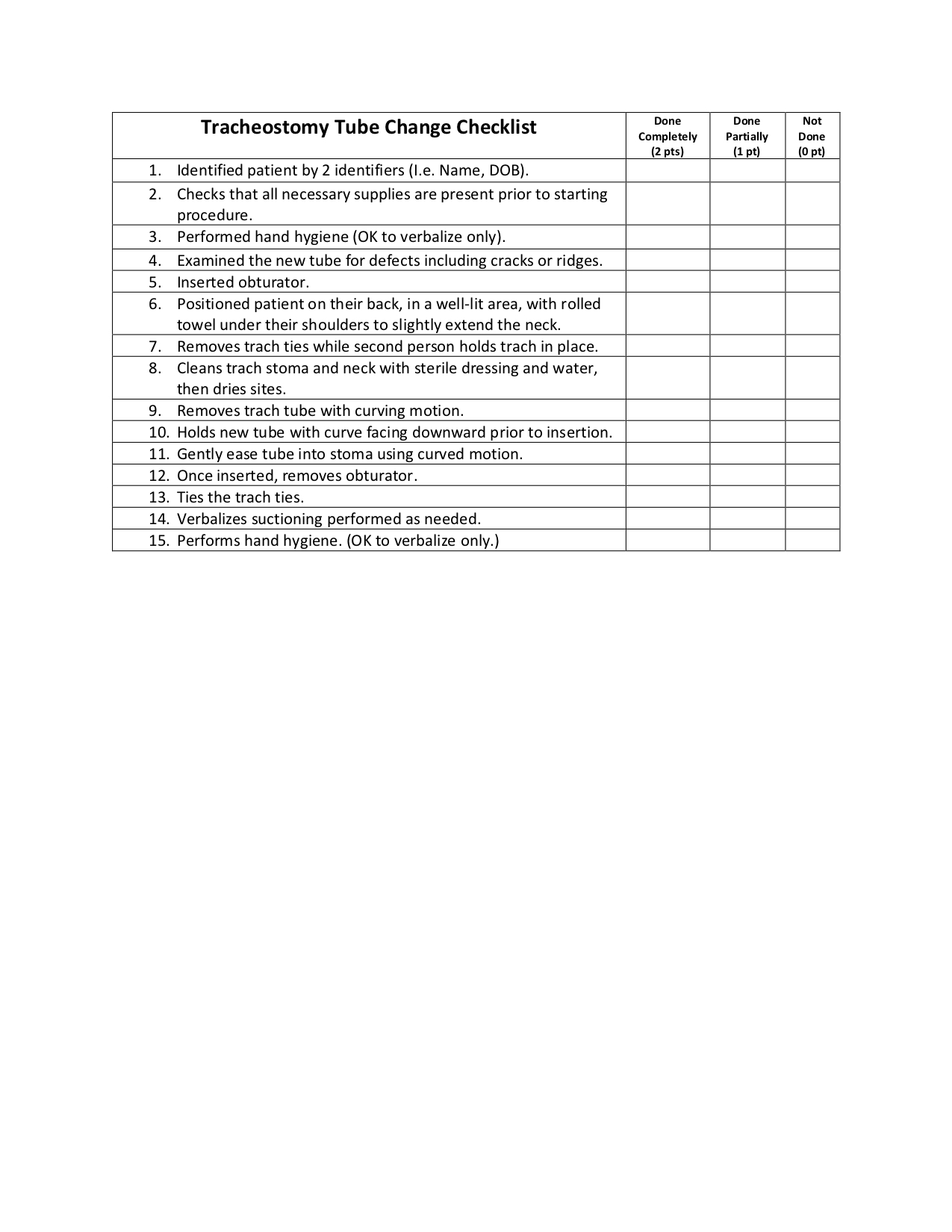
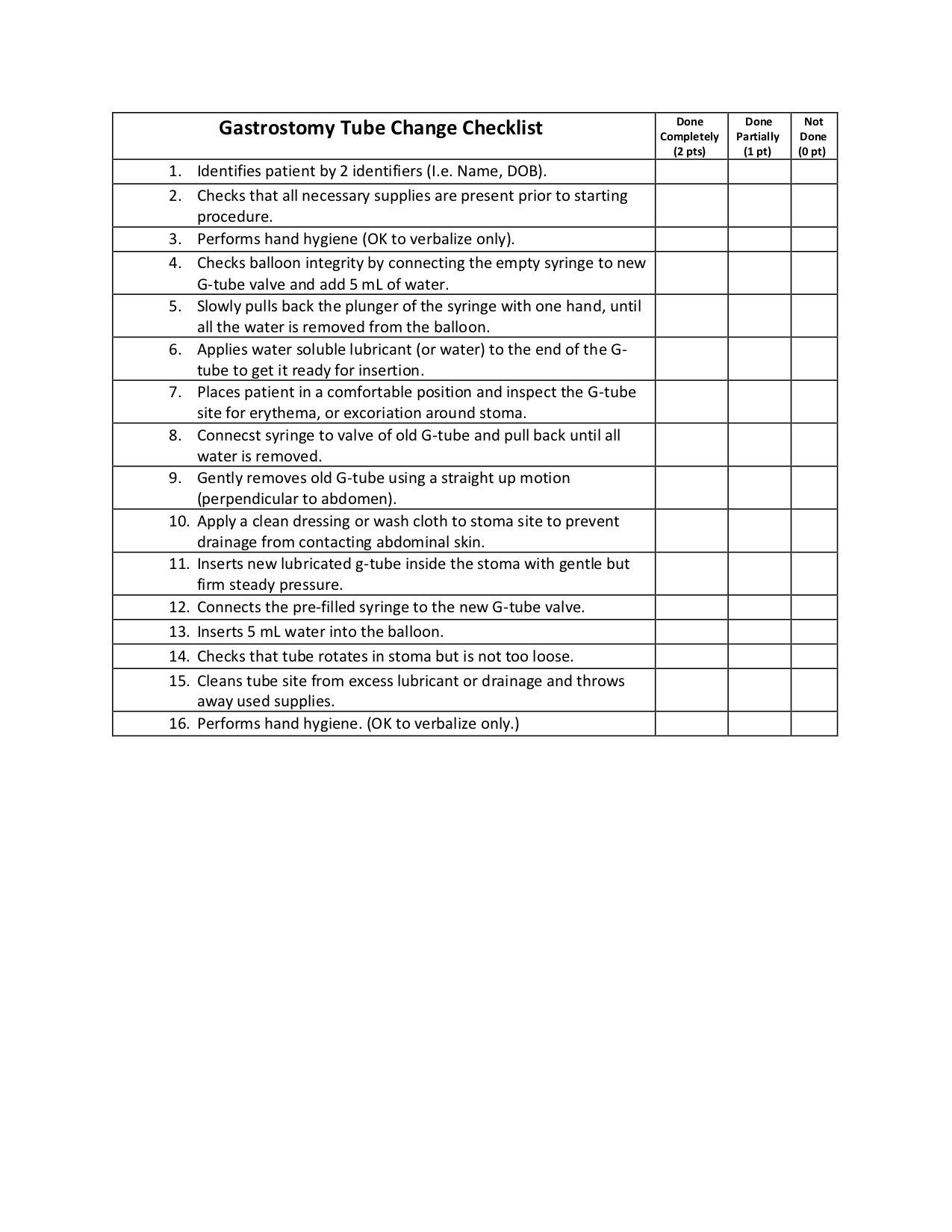
An asynchronous preparatory curriculum included device indications, troubleshooting slides, instructional videos on tube care and changes, and a skills checklist. One-hour group sessions for up to 20 students provided live refreshers, opportunities for questions, and practice led by MD faculty and experienced practitioners. Various models were used for assessment.
Results: All students passed the formative skills evaluation; those initially falling short received immediate feedback and a reattempt opportunity.
Student feedback indicated reduced anxiety when dealing with this patient population and renewed perspectives on bedside procedures. End-of-course evaluations strongly supported integrating these skills.
Conclusion(s): Further monitoring in the academic year 2023-2024 is crucial to assess long-term impact of this innovative formative-only clinical skills assessment.
Aligning curriculum to encompass specific competencies for persons with disabilities across the lifespan is imperative to equip future physicians for this underserved, at-risk population.