Medical Education
Session: Medical Education 1
518 - 'I'm completely off base here on what this child is capable of': A qualitative analysis of how stigma manifests in PICU clinicians' care of children with severe neurological impairment (SNI)
Friday, May 3, 2024
5:15 PM - 7:15 PM ET
Poster Number: 518
Publication Number: 518.63
Publication Number: 518.63

Ellie Oslin, BA (she/her/hers)
Clinical Research Coordinator II
Seattle Children's
Seattle, Washington, United States
Presenting Author(s)
Background: Children with severe neurological impairment (SNI) and their families experience stigma from clinicians, often regarding assumptions about the child’s quality of life and baseline abilities. Clinicians in the pediatric intensive care unit (PICU) face barriers, including time scarcity and heavy workloads that limit their ability to provide personalized care.
Objective: This study examined stigma and strategies to support PICU clinicians in honoring the lives of children with SNI and their families.
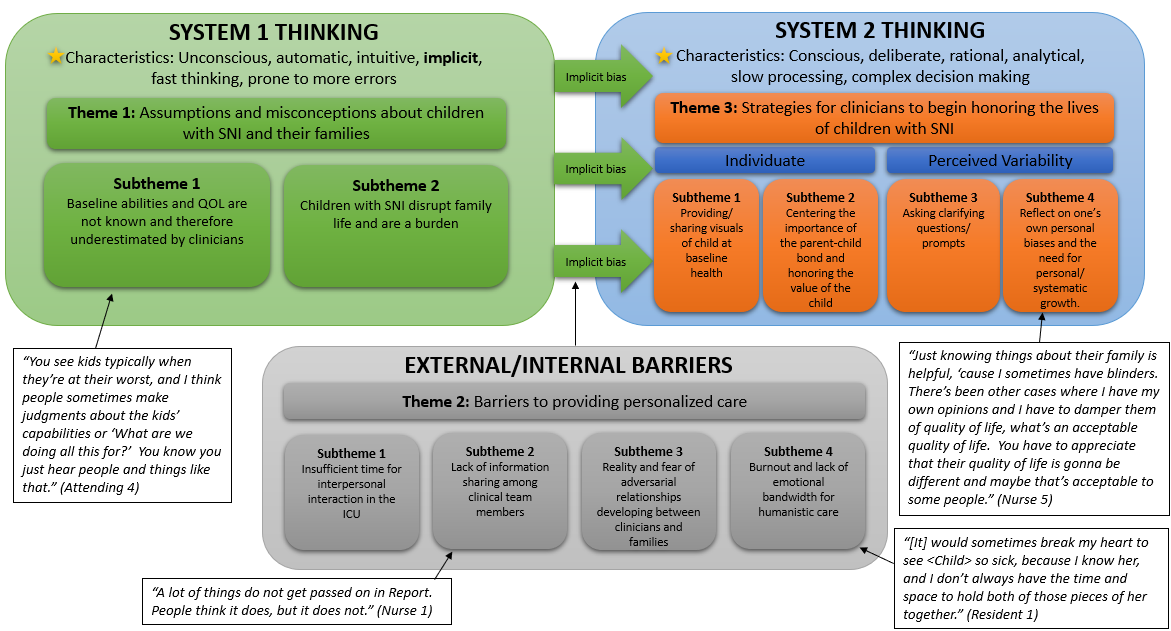
Design/Methods: This qualitative single-center study in the US included PICU clinicians nominated by a child with SNI’s parent/caregiver or purposefully chosen by the study team. Semi-structured 1:1 60-minute interviews were conducted via voice or video call centered on challenges in caring for children with SNI. Audio recordings were professionally transcribed and de-identified before study team coding. Coded data were then extracted, thematically analyzed, and further conceptualized through a bias reduction lens using the dual process theory (DPT) framework.
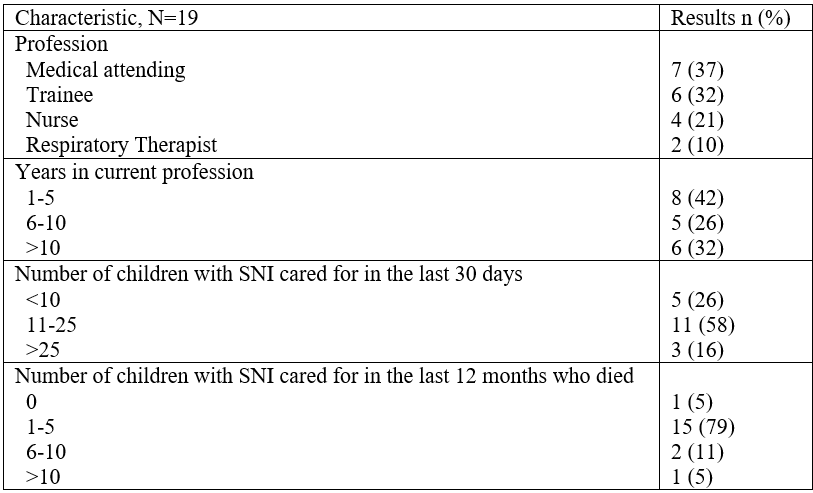
Results: Nineteen PICU clinicians participated: 37% (n=7) medical attendings, 32% (n=6) nurses, 21% (n=4) trainees, and 10% (n=2) respiratory therapists (see Table). Three major themes emerged: 1) assumptions and misconceptions about children with SNI and their families, 2) barriers to providing personalized care, and 3) suggested strategies for clinicians to begin honoring the lives of children with SNI. These aligned with the DPT framework (see Figure). First, system 1 “fast thinking,” occurs when quick observations inform decisions (e.g., clinicians’ snap judgements about what a child is capable of based on their appearance in the PICU). Second, internal and external barriers (e.g., insufficient time for meaningful interpersonal interactions) may prevent clinicians from providing unbiased care. Third, system 2 “slow thinking” where complex decision-making occurs can be enhanced through personalization strategies (e.g., visual depictions of the child’s baseline health, centering family values and clinician reflection on personal biases).
Conclusion(s): This study provides important insights into the challenges and possible strategies for providing personalized care to children with SNI in the PICU. Increasing clinician awareness of their potential implicit biases, how they may be informing care decisions, and the active utilization of bias reduction strategies to mitigate stigma in care are critical areas for future research.