General Pediatrics
Session: General Pediatrics 1
236 - Using QI Methodology to Increase Reach Out and Read Training: A Multi-Site Collaborative
Friday, May 3, 2024
5:15 PM - 7:15 PM ET
Poster Number: 236
Publication Number: 236.67
Publication Number: 236.67
Nathan Sinsheimer, MD
Resident
Duke University School of Medicine
Durham, North Carolina, United States
Presenting Author(s)
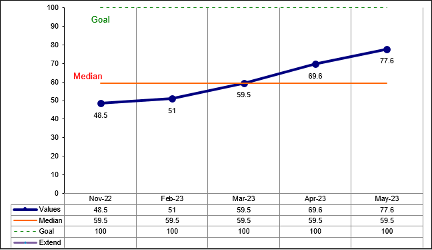
Background: The Carolinas Collaborative (CC) is a network of pediatricians and child health advocates representing the 8 pediatric academic institutions in North and South Carolina. In preparation for piloting a novel Reach Out and Read (ROR) training initiative integrating Emotional Connection (EC) and Early Relational Health (ERH) into the ROR model, clinicians needed to complete the most recent core ROR modules, which contain information required for successful incorporation of EC/ERH into the model. At baseline, 48.5% of clinicians had completed this training.
Objective: Increase ROR core training rates from 48.5% to 100% of current clinicians at all sites within 6 months.
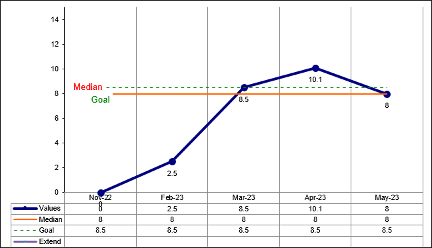
Design/Methods: We assembled an implementation team, including at least one contact from each site. The IHI Model for Improvement with 4 PDSA cycles was used. The team held bi-monthly meetings to share data and approaches to increase training rates. Interventions included connection with ROR affiliates to obtain clinic rosters and generate individual training links, updating rosters, providing structure/creating tools for each site to measure and track their progress, and establishing MOC credit for both the implementation team and additional participants at each site, creating friendly competition and highlighting successful processes so that all sites could use them. The outcome measure of training rates was obtained from the ROR Regional Affiliate's training platform. The process measure was the percentage change in overall training rates to evaluate each intervention's effectiveness. Since the rosters (denominator) changed throughout the study, a more concrete measure, such as number of providers completing the training/number of eligible providers, was not valid.
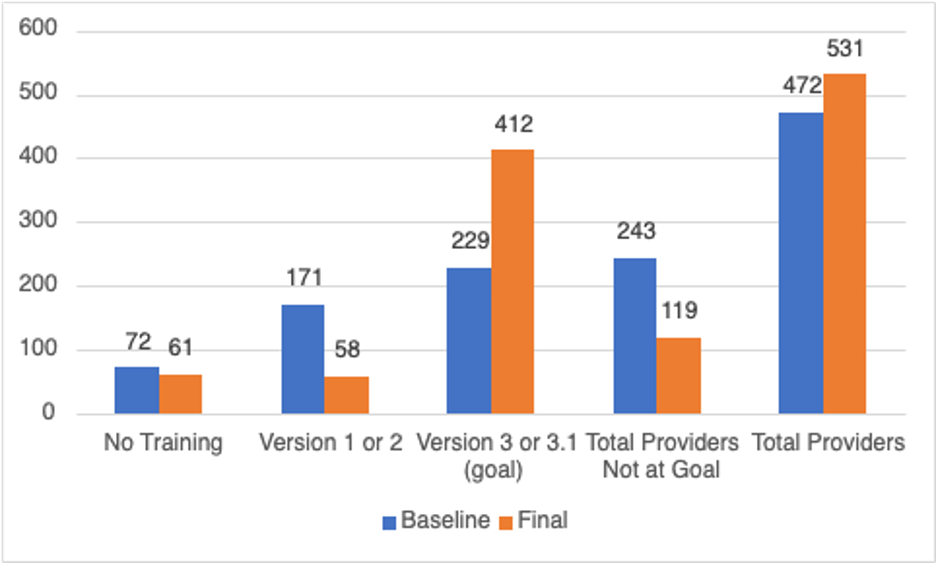
Results: The training rate increased from 48.5% to 51% during the 1st PDSA cycle after the baseline data were initially shared. This increased to 59.5% during the cycle, when the team formally used QI methodology, and to 69.6% during the 3rd cycle when the ability to obtain MOC 4 credit was verified. After the final PDSA cycle of sharing successes and highlighting “bright spots” where training rates were improving above the average, the percentage was 77.6%.
Conclusion(s): There was a dramatic increase in the percentage of providers at goal training. The most successful intervention was formalizing the project as a QI project with an identified leader and offering MOC part 4 credit. Key learning points include maintaining accurate training rosters and highlighting high-performing sites to create friendly competition, team collaboration, and cross-talk between institutions.