Children with Chronic Conditions
Session: Children with Chronic Conditions 1
265 - Supporting children with special health care needs in the medical home
Friday, May 3, 2024
5:15 PM - 7:15 PM ET
Poster Number: 265
Publication Number: 265.72
Publication Number: 265.72

Kitty O'Hare, MD (she/her/hers)
Consulting Associate
Duke University School of Medicine
Cary, North Carolina, United States
Presenting Author(s)
Background: Children and Youth with Special Health Care Needs (CYSHCN) are a diverse population with medical, behavioral, and social needs beyond those of children generally. Within the medical home it can be challenging to identify CYSHCN who are in need of more intense support. Primary Care Providers (PCPs) have different levels of knowledge and skills in coordinating care for CYSHCN.
Objective: In order to better meet the needs of CYSHCN within the medical home, we developed a population health program for our primary care network.
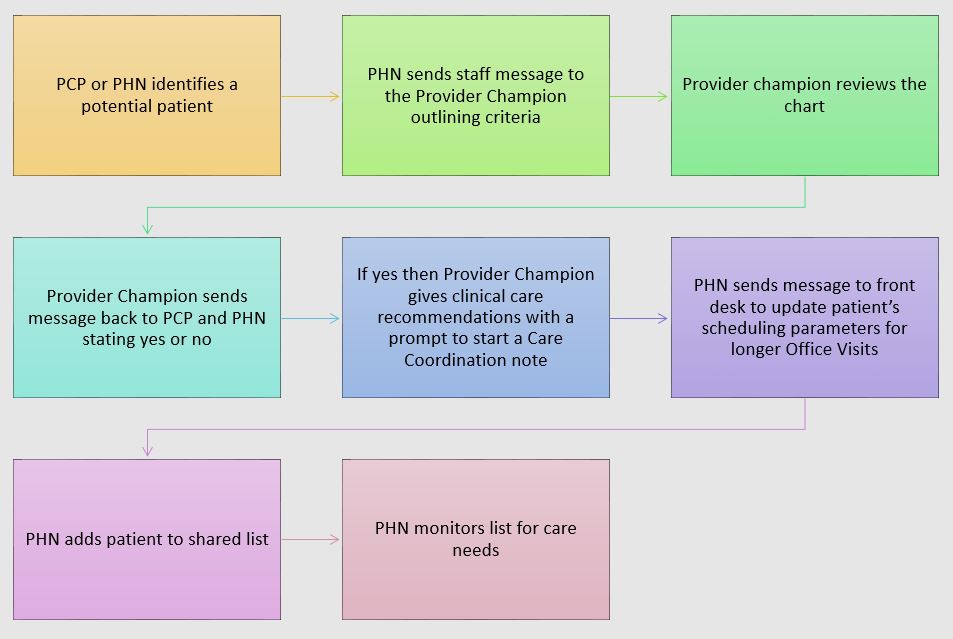
Design/Methods: We designated one general pediatrics practice to trial a CYSHCN program. A population health nurse (PHN) and provider champion (PC) developed inclusion criteria for identifying CYSHCN. These criteria were socialized with the PCPs. Either the PCP or the PHN can identify a patient as meeting criteria, then forward the chart to the PC for review. The PC confirms whether or not the patient meets eligibility criteria, then offers care recommendations back to the PCP / PHN, such as internal referrals (care management, integrated behavioral health, medical-legal partnership) or external referrals (early intervention, Title V programs, Medicaid waivers). The PCP uses these recommendations to develop a Care Coordination Note that is visible to any clinician accessing the chart. Front desk staff modify the scheduling parameters for eligible patients so that they have longer follow-up visits. The PHN tracks CYSHCN on a shared patient list.
Results: In the first 6 months after implementing the program, 45 patients age 0-18 years were added to the CYSHCN list, with a range of 0 to 15 patients per PCP. 26 (57%) are male; 22 (49%) are primarily insured by Medicaid; 5 (11%) have caregivers who speak a language other than English. 20 (44%) have a Care Coordination note. Problem lists include a range of medical diagnoses (e.g. organ transplant) and developmental disabilities (e.g. Trisomy 21); 12 (27%) have a diagnosis of Autism. PCPs report that the eligibility criteria are easy to understand and that the care recommendations are helpful. Overall access to the PCPs, as determined by Third-Next-Available status, was not impacted by offering longer appointments.
Conclusion(s): It is feasible to develop a CYSHCN program within the medical home. In future state we will evaluate outcomes for patients in the CYSHCN program, such as emergency department visits and hospitalizations. We will also evaluate for any disparities in how patients are recommended for the CYSHCN program. We intend to expand this program to other general pediatrics and medicine-pediatrics practices in our network.
.jpg)