Adolescent Medicine
Session: Adolescent Medicine 3
175 - Mitigation of Racial/Ethnic Differences of STI Screening Through Standardized Risk-Derived CDS
Friday, May 3, 2024
5:15 PM - 7:15 PM ET
Poster Number: 175
Publication Number: 175.75
Publication Number: 175.75

Michelle L. Pickett, MD, MS (she/her/hers)
Assistant Professor
Medical College of Wisconsin
Medical College of Wisconsin
Milwaukee, Wisconsin, United States
Presenting Author(s)
Background: As growing data reveal differential treatment of patients based on their race and ethnicity, interventions to mitigate bias in care delivery are needed. One such method is a standardized or automated approach to sexually transmitted infection (STI) screening.
Objective: We sought to determine whether electronic health record (EHR) integrated clinical decision support (CDS) mitigates differential testing of patients based on their race and ethnicity.
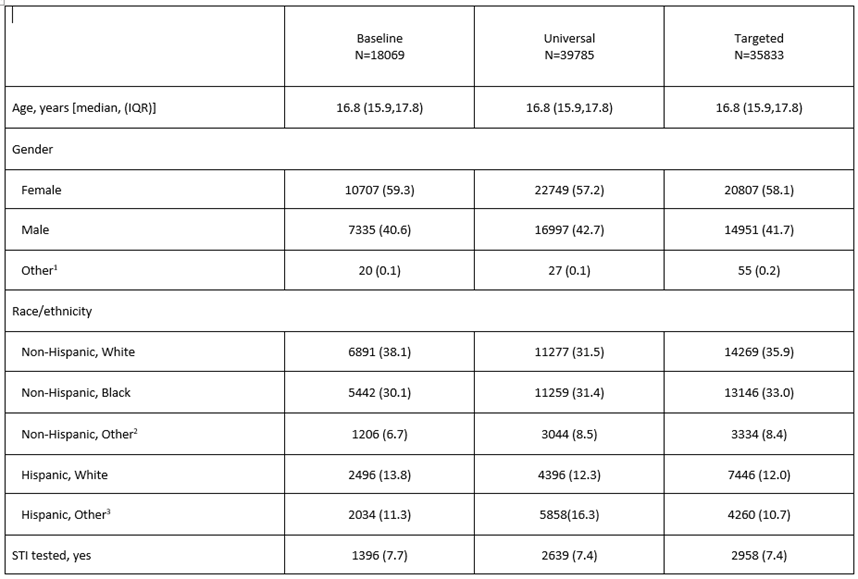
Design/Methods: This is a planned secondary analysis of a prospective pragmatic parent trial at 6 pediatric emergency departments comparing universal vs targeted STI screening in patients aged 15-21 years. Baseline STI testing rates were established. Adolescents completed a tablet-based sexual health screener to determine STI risk. During the universal phase, a patient’s desire for STI testing triggered EHR-embedded CDS. During the targeted phase, the CDS was triggered based on a patient’s STI risk assessment. Racial and ethnic differences with respect to STI testing were compared between phases using a logistic regression model. We also compared the racial and ethnic differences in testing rates between those with CDS alerts and those without, using a separate logistic regression model.
Results: 7.4-7.7% of patients were tested during each study phase (Table 1). During all phases, there were significant differences in testing by race and ethnicity (Fig 1, p< 0.001). During baseline, the largest difference was for non-Hispanic (NH)-Black patients who were more likely to be tested compared to NH-White patients [Baseline OR 2.28 (95% CI 1.99-2.61)]; Hispanic patients were also more likely to be tested [ORs 1.45 (95% CI 1.20-1.75) and 1.64 (95% CI 1.34-2.00) for Hispanic White and Hispanic Other, respectively]. The racial and ethnic differences were not significantly different between intervention phases (Fig 1, p=0.45). In the targeted phase, the interaction between racial and ethnic group and CDS alert was not statistically significant (Fig 2, p=0.25). In the universal phase, racial and ethnic differences were mitigated by the CDS alert (Fig 2, p=0.018).
Conclusion(s): Screening strategies did not have an overall impact on racial and ethnic differences in STI testing across the time periods in which they were carried out. Within the targeted screening phase, the CDS did not mitigate racial/ethnic differences in STI testing. However, in the universal phase the CDS mitigated racial and ethnic differences in STI testing. Further studies exploring racial and ethnic differences are warranted.
.png)
.png)
