Medical Education
Session: Medical Education 8
496 - Resident perceptions of care for children with medical complexity following a non-medical home visit
Monday, May 6, 2024
9:30 AM - 11:30 AM ET
Poster Number: 496
Publication Number: 496.3283
Publication Number: 496.3283

Emily J. Goodwin, MD (she/her/hers)
Associate Professor of Pediatrics
University if Missouri Kansas City School of Medicine, Children’s Mercy Kansas City
Kansas City, Missouri, United States
Presenting Author(s)
Background: Home visiting curricula have been used in medical education to enhance the understanding of medical students and residents regarding patient and family needs outside of the healthcare setting. Pediatric residents from our institution have participated in a non-medical visit to the homes of a child with medical complexity (CMC) since 2009. During the visit, 2-3 residents share dinner with the child and family to learn about their experiences living with and caring for a child with medical complexity and disabilities. After the visit, residents write a reflection prompted by standardized questions and participate in a reflection discussion facilitated by a parent liaison employed by the hospital. During the pandemic, the visits were virtual; in-person visits resumed in July 2023. It is unknown if residents learn similar lessons in the virtual visits compared to the in-person format.
Objective: 1) Explore how a non-medical home visit impacts residents’ perceptions about CMC; 2) Determine if those perceptions differed by visit modality: virtual vs in-person.
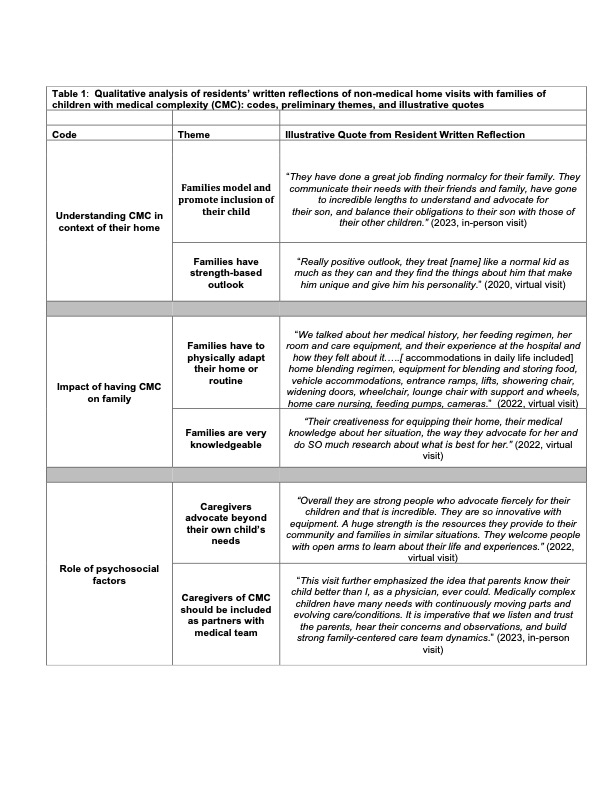
Design/Methods: This qualitative analysis includes 52 written reflections from residents who attended either a virtual or in-person home visit from 2020-2023. We adapted three items from a previously published scale assessing resident’s self-efficacy in understanding components of care as our conceptual framework. This scale characterizes residents’ perceptions of (1) the child in the context of their home, (2) how a child’s needs impact their family, and (3) the role of psychosocial factors in the care of CMC. Using Dedoose software, four authors (including two parent liaisons) coded resident reflections and reviewed code outputs to identify preliminary themes.
Results: Six preliminary themes have emerged regarding resident perceptions of CMC and their families (Table 1): families model and promote inclusion of their child, families have a strength-based outlook, care requires adaptations to the home and routine, families are very knowledgeable, caregivers advocate beyond their own child’s needs, and caregivers are important partners on the care team. These themes appear similar in both virtual and in-person visits in our preliminary analysis.
Conclusion(s): Preliminary findings show that non-medical home visits impact residents’ perceptions of CMC and residents’ understanding of the daily lives of CMC and their families. Additional analyses of the transcripts will be conducted prior to the PAS conference to identify subthemes and further examine if perceptions differ based on visit modality.