Quality Improvement/Patient Safety
Session: Quality Improvement/Patient Safety 3
5 - Improvement of Discharge Communication For General Pediatric Hospitalizations
Monday, May 6, 2024
9:30 AM - 11:30 AM ET
Poster Number: 5
Publication Number: 5.3271
Publication Number: 5.3271

Cindy N. Nguyen, MD (she/her/hers)
Pediatric Hospital Medicine Fellow
Arkansas Children's Hospital
Little Rock, Arkansas, United States
Presenting Author(s)
Background: Misunderstandings in discharge communication, particularly return precautions, are common. Poor discharge communication can result in an increase in patient harm, presentations to the ED, readmissions, and poor patient experience. Written discharge instructions (WDI), when combined with verbal instructions, have been shown to improve communication. Prior studies have shown that improvement of WDI can enhance family comprehension, but few studies have evaluated the impact on patient experience scores.
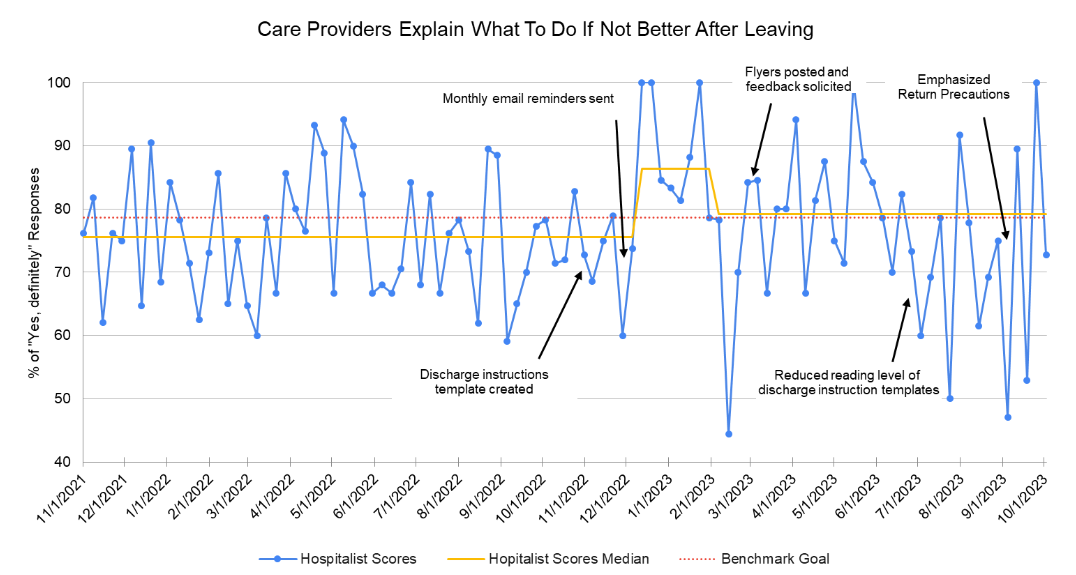
Objective: This project aims to increase the percentage of families of patients admitted to our general pediatrics team who respond “Yes, definitely” to the question, “Did the care providers explain what to do if you did not get better after leaving?” from 75.6% to the national benchmark of 78.6% within one year.
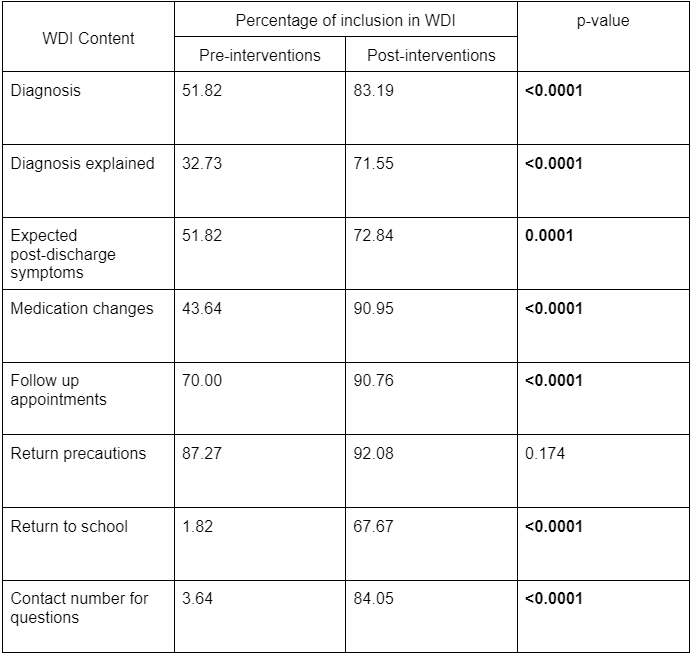
Design/Methods: This quality improvement initiative was conducted at a single, tertiary care pediatric hospital, focusing on families of patients admitted to the general pediatrics teams. Improvement cycles were developed based on literature review: standardization of WDI, written and visual reminders, simplifying the reading level of WDI, and highlighting the return precautions. WDI templates were designed to include several key aspects of discharge instructions including diagnosis, expected post-discharge symptoms, medication changes, follow-up appointments, return precautions, and a number to call with questions. Weekly audits of WDI both before and after interventions were examined and compared for included content using a two-tailed test of proportions. Reading levels were determined using the Flesch-Kincaid Grade level score. Patient experience responses were tracked on a run chart.
Results: Implementation of standardized templates significantly improved how often important content was included in the WDI (Table 1). Introduction of these templates also shifted the percentage of “Yes, definitely” responses from a baseline median of 75.6% to 86.4%. However, after a few weeks, the median shifted down to 79.15%, which is still above the national benchmark. Additional interventions, including decreasing the average reading level from 10.5th grade to 7.5th grade, have not resulted in further shifts.
Conclusion(s): We were able to increase patient experience scores with improvement of our WDI. Interestingly, the majority of our WDI included return precautions prior to our interventions. Formatting and comprehensiveness of the instructions, along with the inclusion of a contact number for questions, may have influenced the perception and effectiveness of the return precautions provided.