Neonatology
Session: Neonatal Quality Improvement 1
383 - Implementation of a PDA Management Algorithm Improves Compliance with PDA Screening and Management Recommendations
Sunday, May 5, 2024
3:30 PM - 6:00 PM ET
Poster Number: 383
Publication Number: 383.1752
Publication Number: 383.1752
- RC
Rehman Chowdhry, MD
Attending Neonatologist
Albany Medical College
Albany, New York, United States
Presenting Author(s)
Background: There is no consensus on clinical or sonographic criteria to determine the need for treatment of a Patent Ductus Arteriosus (PDA) in the preterm infant. The controversy surrounding therapeutic strategy has contributed to wide variation in surveillance and management.
Objective: Implement a PDA Management Algorithm aimed towards improving (1) screening rates and (2) compliance with management recommendations for symptomatic very low birth weight (VLBW) and extremely low birth weight (ELBW) infants from a baseline of 21-63.1% to at least 95% within 12 months.
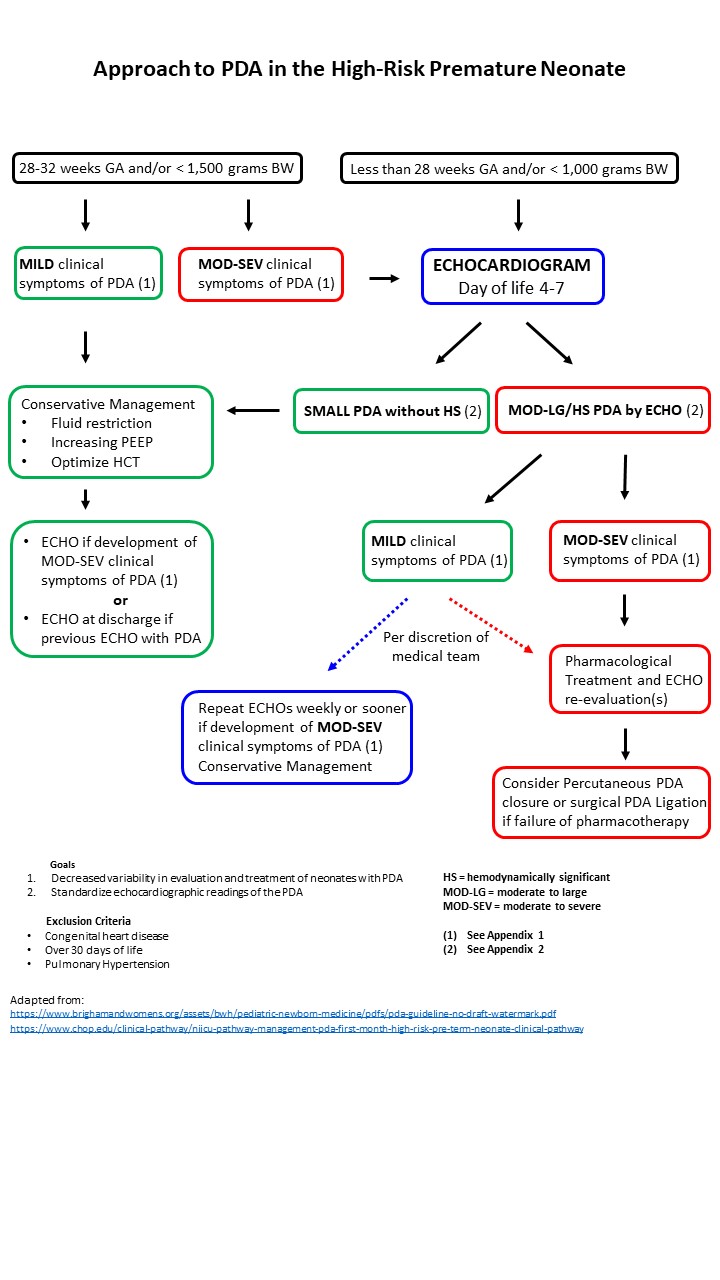
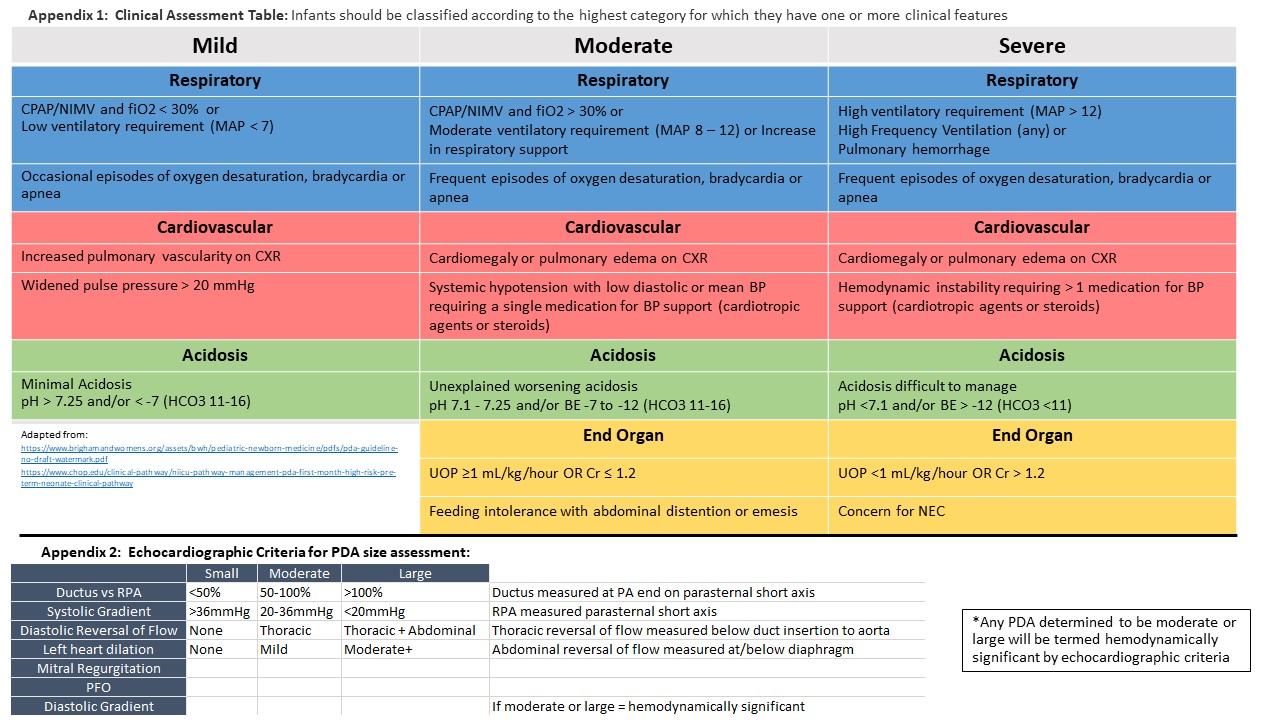
Design/Methods: This quality improvement program (QIP) was conducted at a level IV regional perinatal center with capability for pharmacologic and invasive PDA closure. A multi-disciplinary group of Neonatologists, Pediatric Cardiologists and Advance Practice Providers performed an extensive review of available literature and published guidelines to develop an algorithm that standardized the screening and management of ELBW and symptomatic VLBW infants (Figure 1). These guidelines provided both clinical and echographic criteria to establish the hemodynamic significance of a PDA. (Table 1). This QIP was implemented in January 2022. An educational bundle was developed with planning for PDSA and rapid cycle analyses. Data was collected retrospectively for the year 2021, and then compared to prospectively collected data through the third quarter of 2023 (2023.3).
Results: A total of 181 babies met inclusion criteria for review in this project. The average birthweight was 862g (± 243) and average gestational age at birth was 26.9 weeks (± 2.6). Following implementation, screening rates of ELBWs increased from 63.1% (2021) to 81.1% (2022) to 94.2% (2023.3). Compliance with management recommendations increased from 90.3% (2021) to 95.6% (2022) to 98.4% (2023.3). See control charts (Figure 2). Compliance with recommendation to treat hemodynamically significant PDAs increased from 89.3% (2021) to 95.7% (2022) to 98.5% (2023.3) while overall treatment rates of PDAs decreased from 61.9% (2021) to 53.5% (2022) to 42.9% (2023.3).
Conclusion(s): Implementation of a PDA Management Algorithm improved rates of compliance with screening and management recommendations in the high-risk premature neonate at our institution. Our treatment rates for PDAs determined to be hemodynamically significant increased while overall treatment rates for PDAs decreased since implementation. We continue to collect data prospectively to determine our impact on neonatal morbidities and mortality.
.jpg)
