Neonatology
Session: Neonatal Quality Improvement 3
417 - Improved outcomes in preterm infants with evolving bronchopulmonary dysplasia with implementation of an interdisciplinary BPD program
Sunday, May 5, 2024
3:30 PM - 6:00 PM ET
Poster Number: 417
Publication Number: 417.1757
Publication Number: 417.1757
- MC
Meghan Cusack, MD (she/her/hers)
Resident
Phoenix Children's Hospital
Phoenix, Arizona, United States
Presenting Author(s)
Background: Bronchopulmonary dysplasia (BPD) is one of most common causes of respiratory morbidity in preterm infants and is associated with adverse neurodevelopmental outcomes. Interdisciplinary BPD programs have been shown to improve outcomes in infants with established BPD, however, there are few programs aimed at infants prior to the diagnosis of BPD and few programs at community NICUs. In January 2022, we implemented a BPD program at our level III community hospital which consists of weekly interdisciplinary team rounds inclusive of neonatologists, pulmonologists, nurses, dieticians, physical, occupational, speech and respiratory therapists and families identifying infants at 32 weeks corrected gestation at risk for the development of BPD.
Objective: The objectives of the program were to decrease length of stay, incidence of severe BPD, and need for transfer to quaternary center for tracheostomy evaluation in preterm infants at risk of developing BPD.
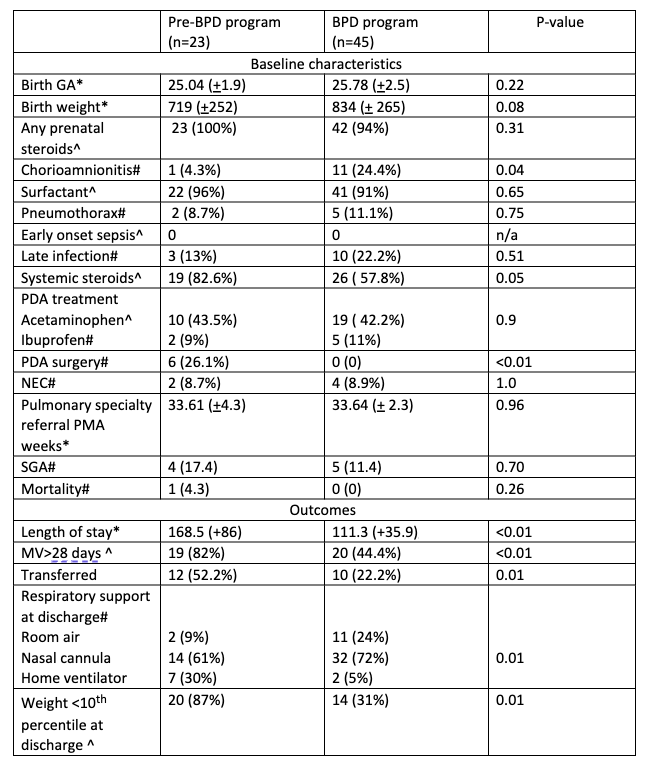
Design/Methods: This was a retrospective cohort study of preterm infants born before 32 weeks and referred to a pulmonology specialty team. We compared baseline maternal and infant characteristics and outcomes, including length of stay (LOS), need for mechanical ventilation greater than 28 days, respiratory support at discharge, and proportion of infants with discharge weight < 10th percentile for two epochs of care; prior to implementation of program (pre-BPD program, 2020-2021) and post implementation (BPD program,2022).
Results: A total of 68 infants were included in the study (n=23; Pre-BPD program and n=45; BPD program). Baseline characteristics were similar between the two cohorts except for higher proportion of infants born with maternal chorioamnionitis in the BPD program cohort (24.4% vs 4.3%, p 0.04) (Table 1). Infants in the BPD program cohort had shorter LOS (113 vs 168 days, p< 0.01) and lower proportion of infants requiring mechanical ventilation greater than 28 days (44.4% vs 82%, p< 0.01). A higher proportion of infants were discharged home on room air and nasal cannula in BPD program and lower proportion requiring home ventilatory support (p= 0.01). Infants in the BPD program had lower proportions of infant with discharge weight below 10th centile (31% vs 87%; p< 0.01).
Conclusion(s): Implementation of an interdisciplinary BPD program in preterm infants at risk of BPD at our level III community NICU was associated with improved outcomes in length of stay, need for transfer and home with ventilatory support and discharge weight. Larger multi-center collaborative studies with long-term follow-up are needed to further validate our results.