Adolescent Medicine
Session: Adolescent Medicine 3
173 - Identifying Provider Attitudes, Practices, and Barriers to Three-Point Extra-Genital Testing for Neisseria Gonorrhea and Chlamydia Trachomatis Infections Among Adolescents and Young Adults
Friday, May 3, 2024
5:15 PM - 7:15 PM ET
Poster Number: 173
Publication Number: 173.106
Publication Number: 173.106
James T. DeCuir, Jr. (he/him/his)
Medical Student
Baylor College of Medicine
Houston, Texas, United States
Presenting Author(s)
Background: The prevalence of Neisseria gonorrhea (GC) and Chlamydia trachomatis (CT) infections has been rising nationally, particularly among young individuals. In 2020, almost 2/3 of CT infections occurred in 15–24 year-olds, and GC infections have increased by 111% since 2009. The CDC recommends universal screening for CT and GC in sexually active women under 25 and men who have sex with men, with screening in men who have sex with women based on risk factors. However, adolescents are often under-screened, and compounding the issue, screening rates decreased during the COVID-19 pandemic.
Objective: This study aims to investigate provider attitudes, knowledge and practices regarding recommended sexually transmitted infection (STI) testing, focusing on extra-genital screening for GC and CT in a large urban pediatric hospital system.
Design/Methods: Pediatric providers (residents, fellows, attendings, and advanced practice providers (APPs)) in primary care, urgent care, emergency room, and inpatient settings were anonymously surveyed via REDCap (n=599). The surveys were distributed using hospital listservs and addressed provider attitudes towards sexual history taking and STI screening, knowledge and practice of three-point testing (throat, genital, and anal), and barriers to testing.
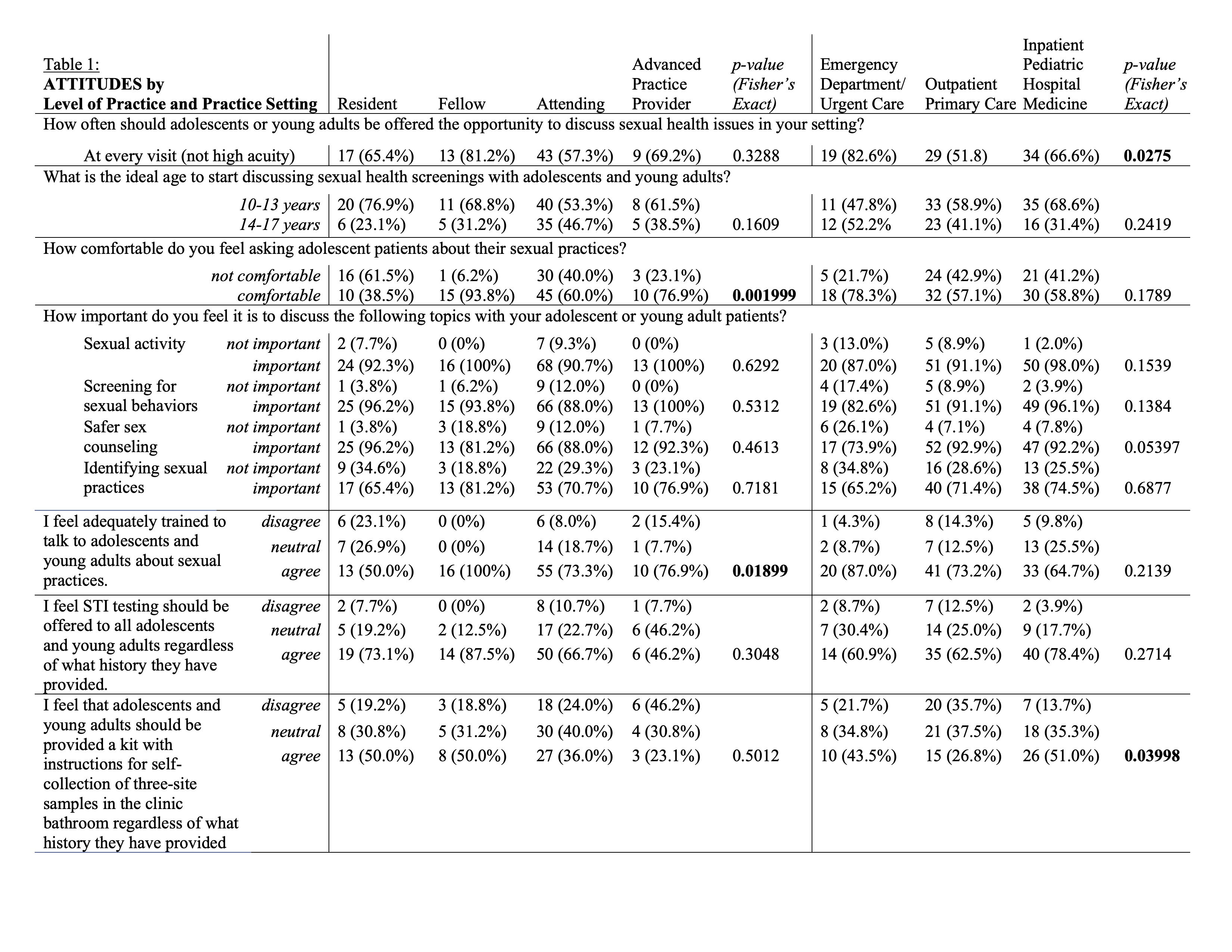
Results: Fisher-exact tests were used to compare the 130 completed responses based on provider level and practice setting. Providers reported discomfort asking adolescents about their sexual practices (61.5% of residents & 40% of attendings, p=0.002), though a minimum of 65.4-88% agreed that these were important to discuss. Only 50% of residents and 73.3% of attendings felt adequately trained to discuss sexual practices (p=0.02). 30.8% of residents and 36.0% of attendings were unlikely to counsel patients on safer sex practices. Half of residents and attendings were unlikely to ask about patients’ sexual orientation. Only 30.8% and 48% of attendings and APPs knew that either providers or patients can collect extra-genital samples. Over 90% of outpatient and inpatient providers faced barriers to three-point testing, including confidentiality concerns, lack of swabs, and knowledge gaps.
Conclusion(s): Provider comfort level with discussions of sexual health practices was low in our study. Knowledge and acceptability of self-collection for extra-genital specimens was not uniform. Notable barriers include confidentiality concerns and logistical challenges. Addressing these barriers may enhance screening rates and reduce missed opportunities for STI care among adolescents and young adults across multiple healthcare settings.
.jpg)
.jpg)
