Medical Education
Session: Medical Education 4
392 - Determining the Effectiveness of an ‘Outpatient Procedures and Emergencies in the Primary Care Setting’ Curriculum for Differentiated Senior Medical Students
Saturday, May 4, 2024
3:30 PM - 6:00 PM ET
Poster Number: 392
Publication Number: 392.1599
Publication Number: 392.1599

Helen C. Wang, MD (she/her/hers)
Associate Clinical Professor
UCSD
La Jolla, California, United States
Presenting Author(s)
Background: The majority of pediatric residency graduates will practice outpatient general pediatrics. Although pediatricians regularly treat patients with urgent conditions, only 50% feel prepared to manage common outpatient emergencies. This gap in preparedness has consequences on patient safety and quality of care, especially in areas where access to care is limited. Few existing MedEd curricula focus on teaching outpatient pediatric emergency and procedure skills at both the undergraduate and graduate medical education level. Our course attempts to address this at an early stage of training, focusing on providing education to rising Pediatric, Med-Peds, and Family Medicine interns, to allow for scaffolding to occur as they progress through residency.
Objective: Increase differentiated senior medical students’ confidence in managing outpatient pediatric emergencies and performing outpatient pediatric procedures.
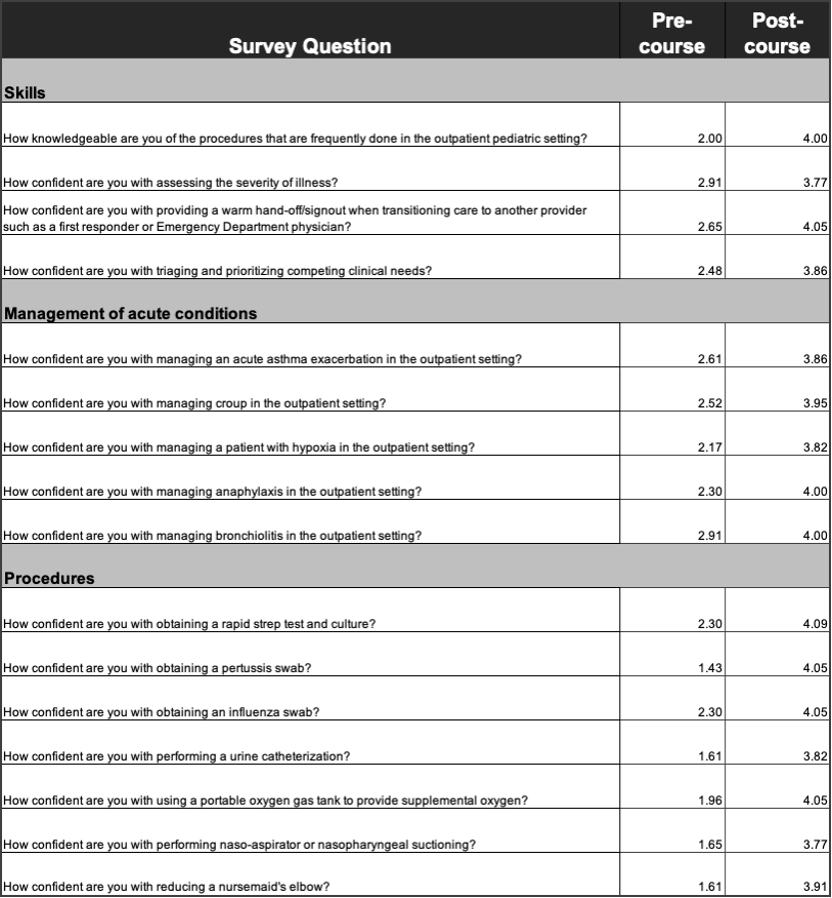
Design/Methods: Through role play and guided reflection by four trained facilitators, medical students participated in a 2 hour long course involving 9 primary care cases with 19 unique learning objectives and procedures. Cases included management of croup, hypoxia, anaphylaxis, bronchiolitis, and acute asthma exacerbation. Procedural skills included reducing a nursemaid’s elbow, practicing urinary catheterization, performing naso-aspirator/nasopharyngeal suctioning, providing supplemental oxygen, and swabbing for strep, pertussis, and influenza. Participating students completed a survey before and after the session. Data was analyzed using SPSS to determine effectiveness and to refine the curriculum.
Results: A total of 23 fourth-year medical students entering Pediatrics, Med-Peds, or Family Medicine residency participated. For each of the 19 unique learning objectives, participants felt more confident after the course.
Conclusion(s): This course increased senior medical students’ confidence in identifying and managing outpatient pediatric emergencies and in performing outpatient pediatric procedures. The strengths of this course include its effectiveness and low implementation costs in terms of materials and facilitators. Through this curriculum, we hope to better prepare physicians, especially those practicing in low resource communities, to manage and stabilize patients who require procedures or present with emergent concerns. Future directions include: adding additional simulation scenarios, implementation at other academic institutions, and tracking the longitudinal impact on participants’ confidence levels with outpatient procedures and emergencies as they progress through residency and beyond.