Critical Care
Session: Critical Care 2
124 - Epidemiology of Hospitalizations and Outcomes in Pediatric Hepatic Encephalopathy
Monday, May 6, 2024
9:30 AM - 11:30 AM ET
Poster Number: 124
Publication Number: 124.3248
Publication Number: 124.3248
- fO
folafoluwa Odetola, MB ChB, MPH (he/him/his)
Associate Professor
University of Michigan Medical School
Ann Arbor, Michigan, United States
Presenting Author(s)
Background: Pediatric acute liver failure is a potentially life-threatening disease, particularly with the occurrence of hepatic encephalopathy (HE), a harbinger of adverse patient outcomes. HE precludes objective clinical neurologic examination and often prompts deployment of multimodal clinical approaches to mitigate elevated intracranial pressure and other concurrent or emerging non-hepatic organ system dysfunction.
Objective: To test the hypothesis that multiple organ dysfunction (MOD) among hospitalized children and adolescents with HE will be associated with mortality.
Design/Methods: Retrospective cohort study of children 0-20 years old hospitalized with HE, using combined data from the 2016 and 2019 versions of the Kids’ Inpatient Database. National estimates of hospitalizations were generated, and multivariate analyses conducted to determine patient and hospital characteristics independently associated with mortality.
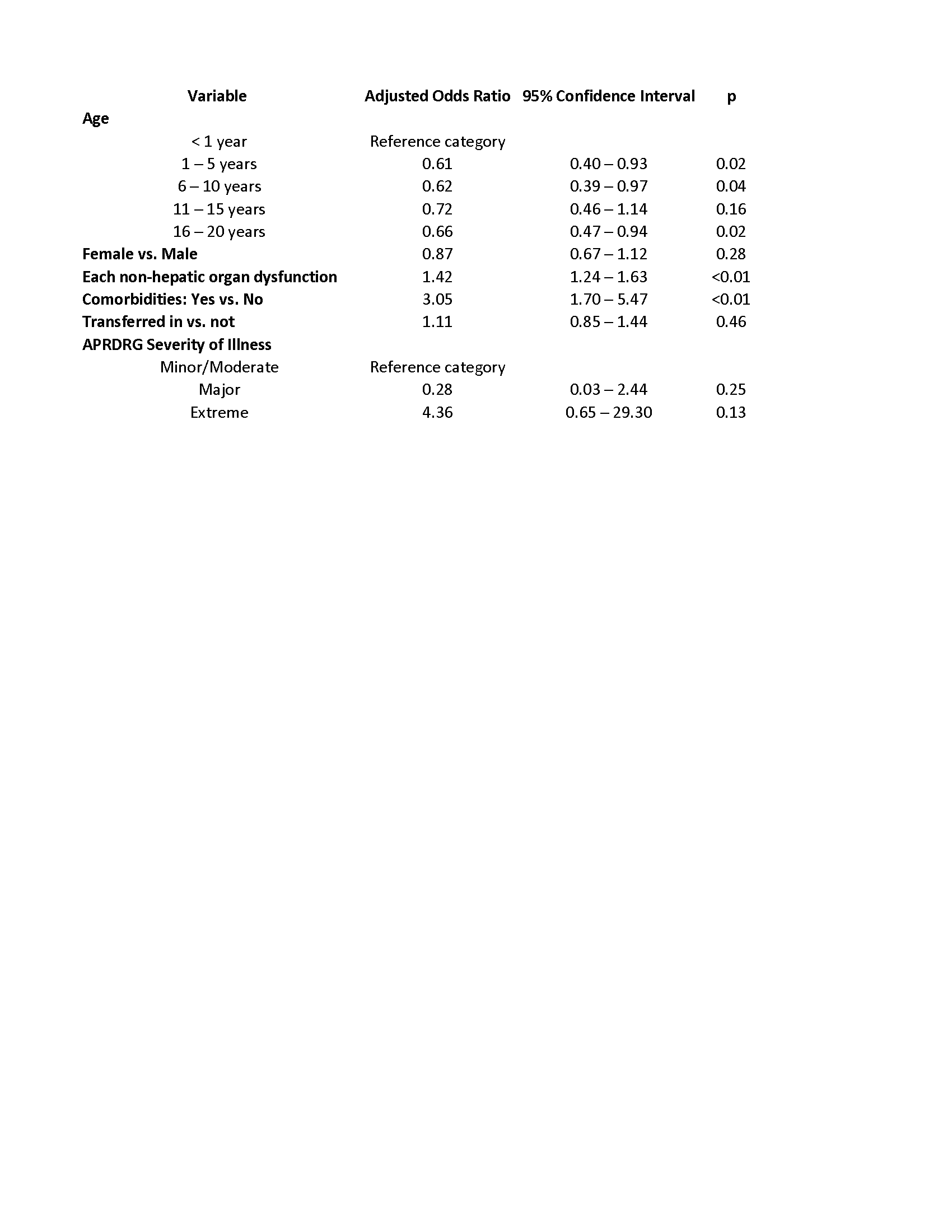
Results: Of an estimated 1,638 hospitalizations nationally for pediatric HE, most (94%) were to urban teaching hospitals, 66% were > 5 years, and 56% were male. Comorbidities were present in 93% of children, 97% had multiple organ dysfunction (MOD), and 91% had extreme illness severity. In-hospital mortality was 42%, average hospital stay was 22 days, and average hospital charge was $563,534. Intracranial pressure monitoring occurred in 46 (3.8%) of patients, and 21(1.8%) underwent liver transplantation. Mortality was not associated with gender, payer type, or hospital characteristics, including bed side, census region, or type of hospital. Infancy, MOD, and the existence of comorbidities were associated with in-hospital mortality (Table).
Conclusion(s): Nearly 1 in 2 children with hepatic encephalopathy succumbed to their illness. The care of these critically ill children occurs predominantly at urban hospitals, with no regional or hospital variation in mortality. Efforts to mitigate mortality need to be individualized, with emphasis on alleviating or preventing MOD.