Nephrology
Session: Nephrology 3
2 - Addition of Urine NGAL to Serum Creatinine Improves Prediction of Cefepime Clearance in Pediatric ICU Patients at High Risk of Acute Kidney Injury (AKI)
Sunday, May 5, 2024
3:30 PM - 6:00 PM ET
Poster Number: 2
Publication Number: 2.1778
Publication Number: 2.1778
- HH
H. Rhodes R. Hambrick, MD
Fellow in Nephrology and Hypertension
Cincinnati Children's Hospital Medical Center
Cincinnati, Ohio, United States
Presenting Author(s)
Background: Cefepime (FEP) is commonly used for empiric treatment of sepsis in the Pediatric ICU (PICU). FEP undergoes renal clearance (CL), requiring dose-adjustment with changes in kidney function. Serum creatinine (SCr) is typically used to estimate glomerular filtration rate (eGFR), though SCr changes are delayed relative to changes in actual GFR. Urine neutrophil gelatinase-associated lipocalin (uNGAL) is a marker of tubular injury and can be elevated prior to changes in SCr. uNGAL is ordered automatically in our PICU when patients are at elevated risk of AKI based on a renal angina index (RAI, an AKI risk prediction score) of >=8. It is unknown if uNGAL is useful in predicting changes in FEP CL earlier than changes in SCr.
Objective: To determine if inclusion of uNGAL improves prediction of FEP CL in PICU patients at risk of AKI.
Design/Methods: We prospectively enrolled patients admitted to the PICU with RAI of >=8, prescribed FEP and not receiving extracorporeal therapy. FEP concentrations were measured from residual blood obtained from scavenged opportunistic samples. We analyzed plasma FEP concentrations using pharmacokinetic (PK) modeling software (MwPharm++, Mediware) and a pediatric FEP PK model to estimate FEP CL. We used linear regression to compare uNGAL, SCr-eGFR (defined by bedside Schwartz for patients < 18 and by race-neutral CKD-EPI equations for patients ≥18), and SCr-defined AKI as predictors of FEP CL normalized to body surface area (BSA) before and after 48h post-PICU admission (b48h/a48h).
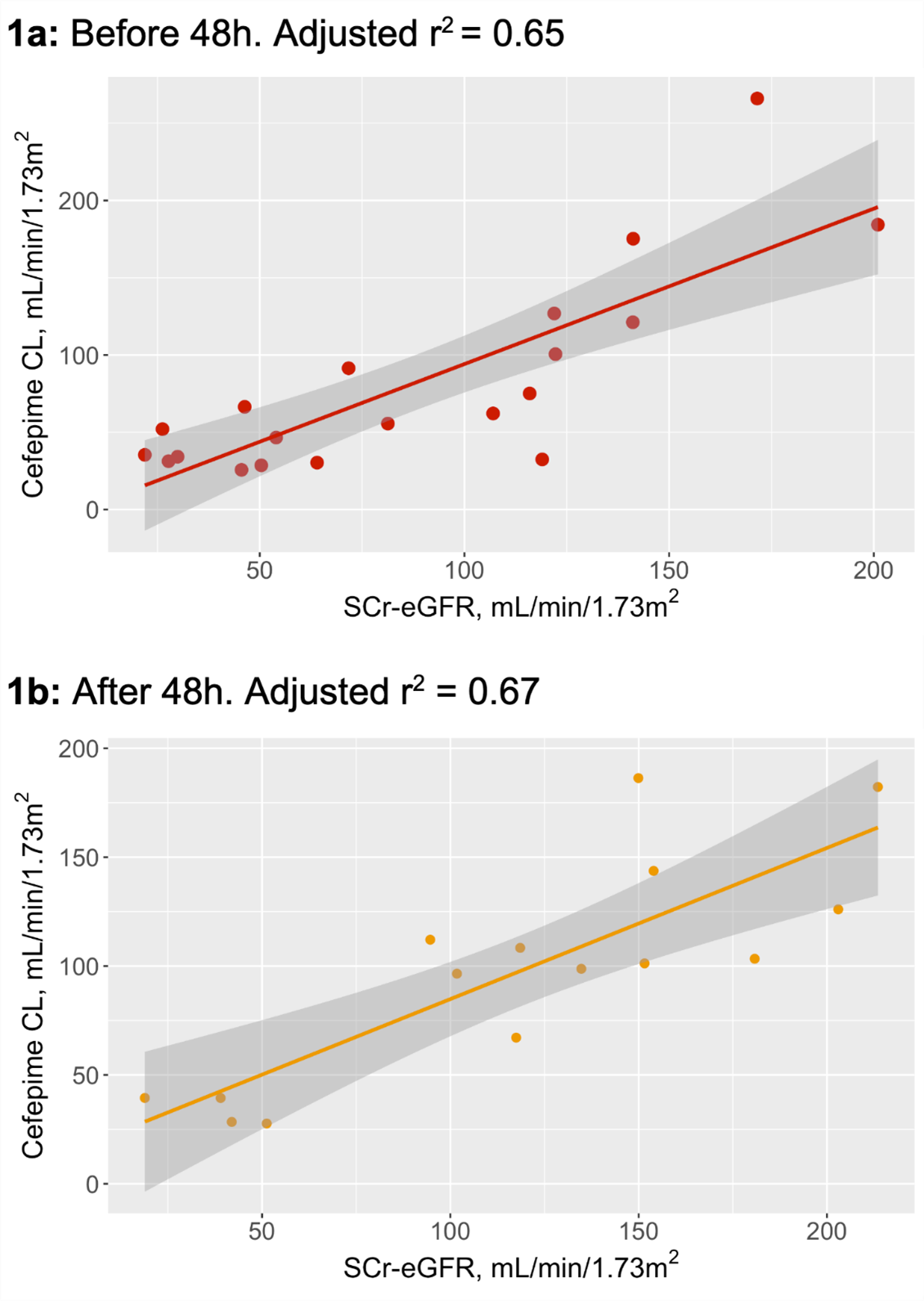
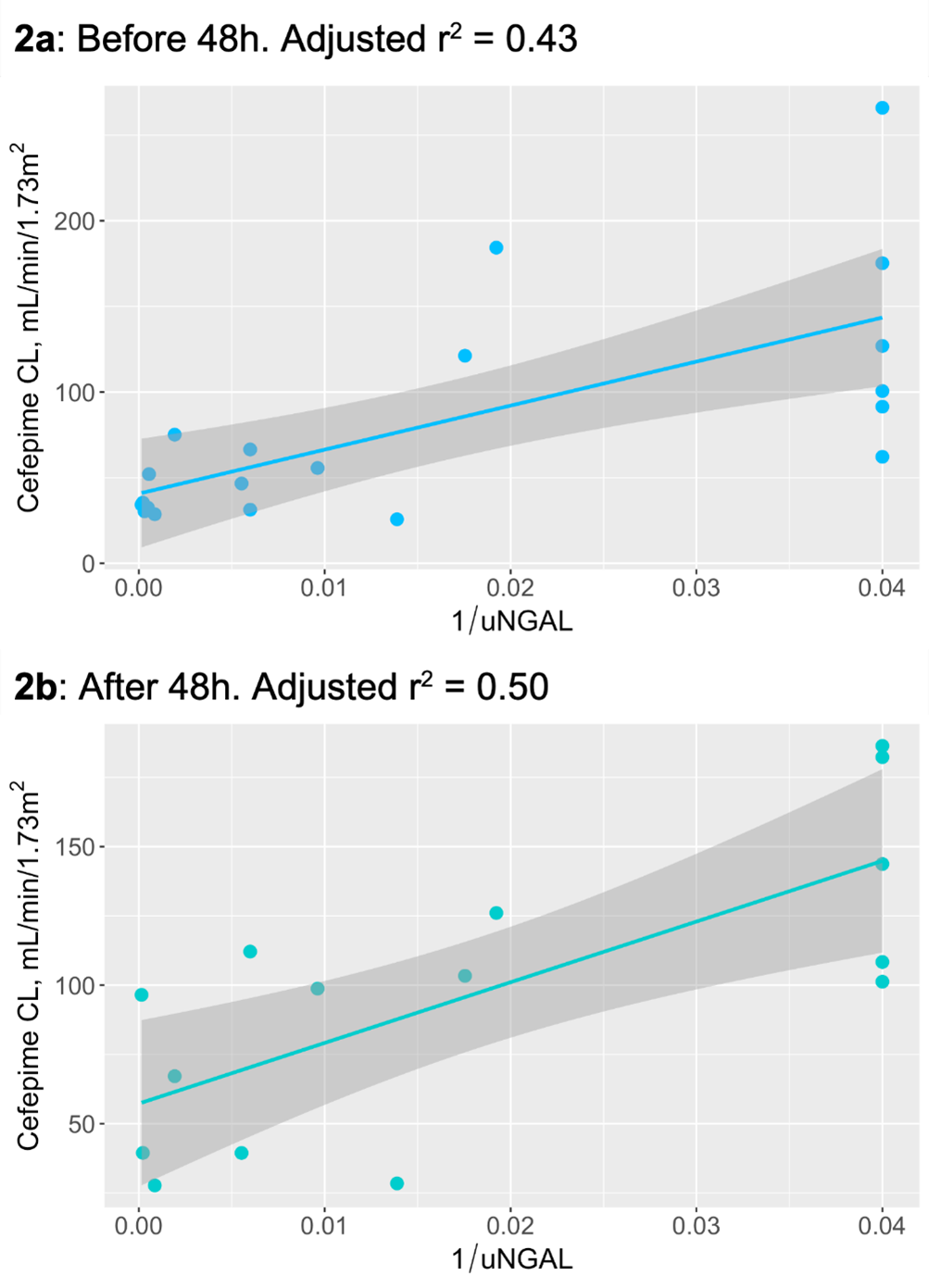
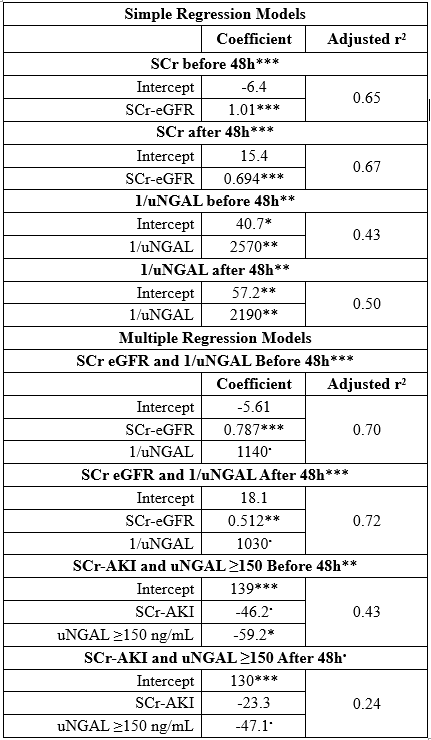
Results: 20 patients (age range 0.3-26.6 yr, mean 11.6, 50% female) were included. Patients had 4-9 FEP concentrations available for analysis; 15 (75%) had concentrations available a48h. Twelve (60%) had SCr-defined AKI on PICU admission and 10 (50%) had elevated uNGAL using accepted threshold of 150 ng/mL. In univariate analyses, SCr-eGFR was associated with FEP CL b48h (adjusted [a]r2=0.65) and a48h (ar2=0.67) (Figure 1a-b). uNGAL values were skewed so the geometric inverse was used; 1/uNGAL was associated with FEP CL b48h (ar2=0.43) and a48h (ar2=0.50) (Figure 2a-b). In multivariable linear regression, combining SCr-eGFR and 1/uNGAL improved model performance with ar2=0.69 (b48h) and 0.72 (a48h) (Table 1). In a separate multivariable model, elevated uNGAL (150 ng/mL) was associated with a ~40% decrease in FEP CL after controlling for SCr-AKI (Table 1).
Conclusion(s): uNGAL concentrations at PICU admission are associated with decreased FEP CL b48h and a48h. Addition of uNGAL to SCr-eGFR-based models of FEP CL may improve prediction of cefepime CL compared with SCr-eGFR alone.