Medical Education
Session: Medical Education 2
533 - Mixed Method Evaluation of Neonatal-Perinatal Medicine Fellowship Advanced Airway Curricula & Assessment Techniques
Friday, May 3, 2024
5:15 PM - 7:15 PM ET
Poster Number: 533
Publication Number: 533.130
Publication Number: 533.130

Mark R. Castera, MD (he/him/his)
Neonatal-Perinatal Medicine Fellow
Childrens Hospital of Philadelphia
Philadelphia, Pennsylvania, United States
Presenting Author(s)
Background: Many incoming Neonatal-Perinatal Medicine (NPM) fellows have limited tracheal intubation (TI) exposure at the start of fellowship due to reduced TI opportunities during residency training. This puts increased pressure on NPM training programs to optimize their trainees’ TI experience during fellowship as TI competency is an ACGME graduation requirement. A prior survey of NPM programs showed significant variability in educational curricula, assessment techniques, & resources for TI training. The optimal training structure to support TI competency development is unknown.
Objective: In-depth exploration of NPM fellowship TI education & assessment practices with fellowship leaders using qualitative research methods
Design/Methods: To further explore results from a recent survey on TI training of NPM fellowship leaders, a semi-structured interview guide was designed to conduct in-depth, qualitative interviews with NPM fellowship leaders regarding their TI educational practices. Interview questions were created to explore themes identified from prior survey data. Semi-structured interviews were conducted via MS Teams. Using principles of grounded theory, interviews were transcribed & thematic analysis was performed using nVIVO coding software.
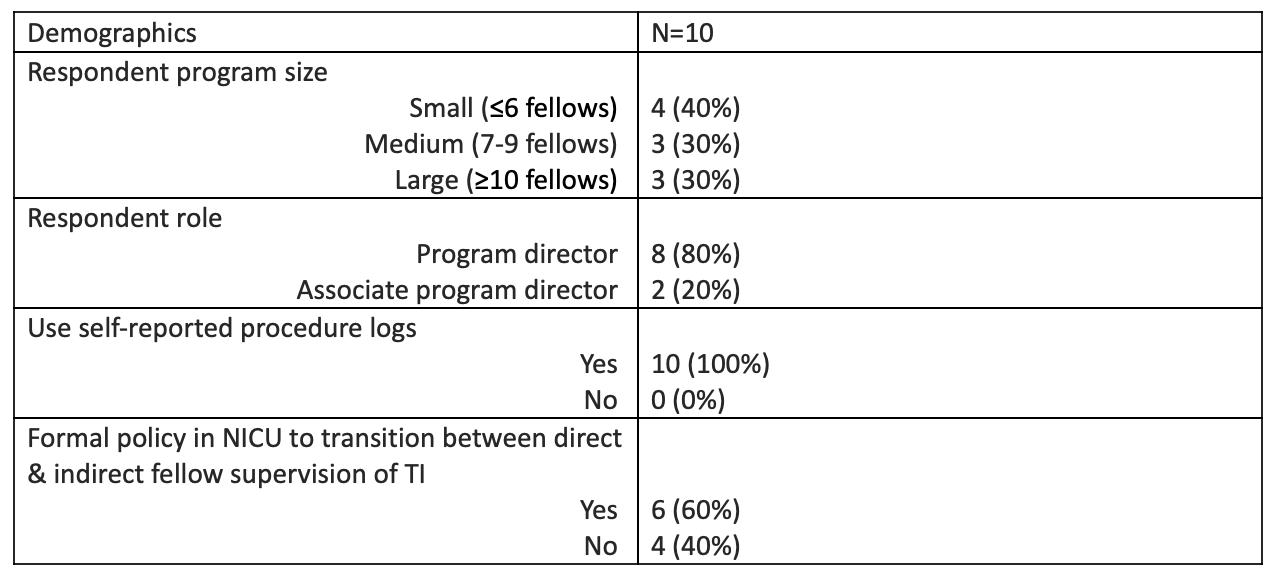
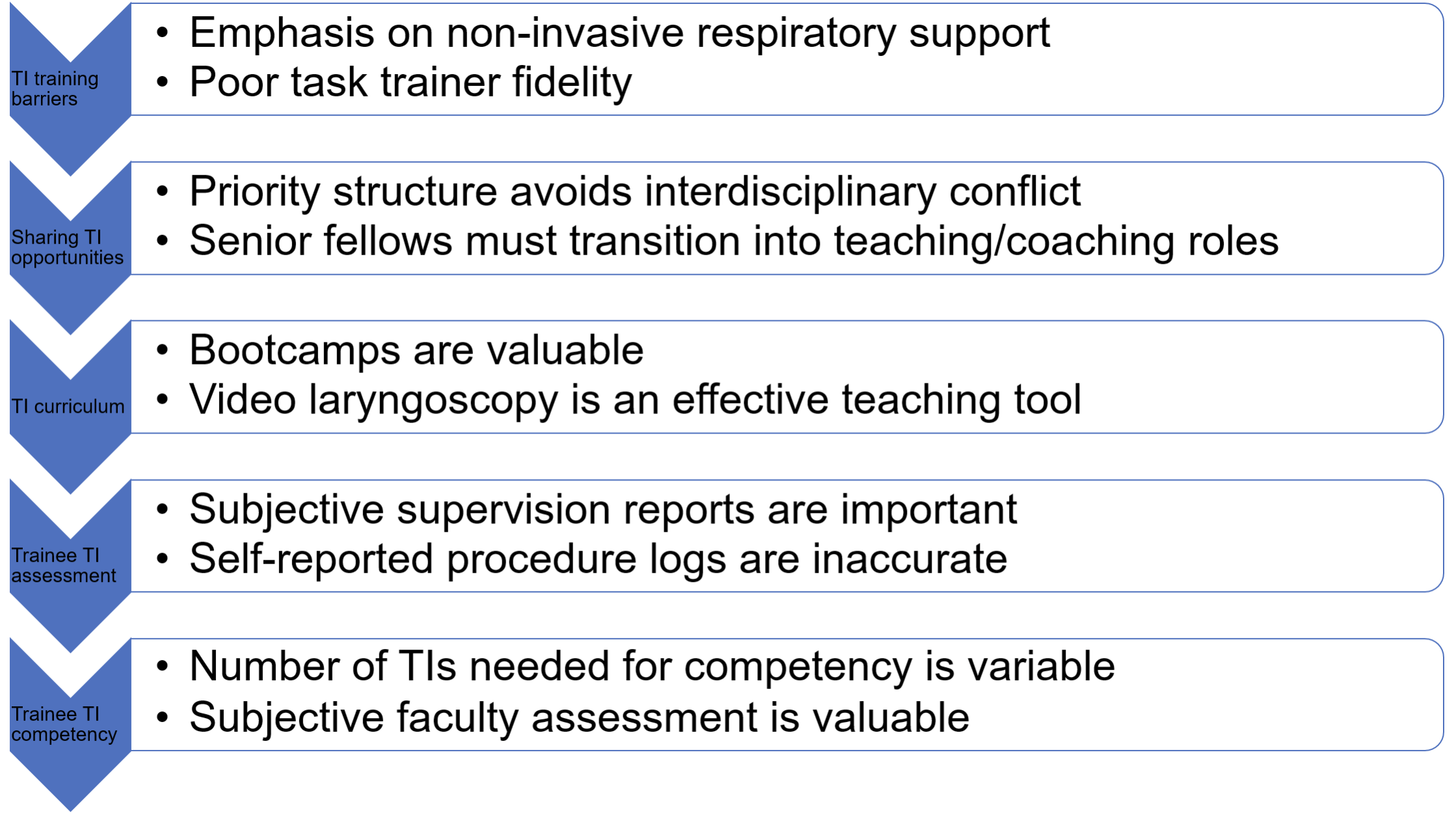
Results: Table 1 shows participant demographics. Thematic saturation was reached after 10 interviews. Table 2 demonstrates common themes & subthemes with representative quotes. Key points from thematic analysis of the interviews are shown in Figure 1. Many educators reported that while simulation is a valuable tool to support TI competency development, primary learning comes from clinical experience. Most educators acknowledged that qualitative faculty observations are a valuable measure of TI competency & assigning a minimum number of TI encounters as a proxy for competency is not valuable.
Conclusion(s): TI education is a challenging educational component for NPM fellowship programs. In this study, educators report that limited TI procedural opportunities & competition between fellows & other NICU airway providers for TIs are concerns. Bootcamps, simulated TI experiences, & structured priority systems for TI attempts can help to mitigate these issues. Many educators feel video laryngoscopy has helped accelerate their fellows’ procedural competency by providing more specific feedback to fellows. NPM educators view self-reported procedure logs with skepticism & often base their TI competency assessments on subjective reports. Future investigation is needed to determine which TI educational & assessment practices are associated with improved clinical performance.
.png)
