Global Neonatal & Children's Health
Session: Global Neonatal & Children's Health 3
501 - A Characterization of Pediatric Burn Injury Patients Presenting to an Emergency Department in Northern Tanzania
Friday, May 3, 2024
5:15 PM - 7:15 PM ET
Poster Number: 501
Publication Number: 501.138
Publication Number: 501.138

Kajsa Vlasic, MD (she/her/hers)
Pediatric Emergency Medicine & Global Health Fellow
University of Utah School of Medicine
Salt Lake City, Utah, United States
Presenting Author(s)
Background: Burn injuries disproportionately impact children in low- and middle-income countries (LMICs), with the highest incidence in Sub-Saharan Africa. While high mortality rates due to burn injury in pediatric patients in LMICs have been identified, there is limited information characterizing this population upon arrival to the emergency department (ED).
Objective: This study aimed to describe the pediatric burn injury population presenting to the ED of a tertiary referral hospital in Northern Tanzania. We evaluated how factors from ED presentation were associated with level of hospital care, morbidity, and in-hospital mortality.
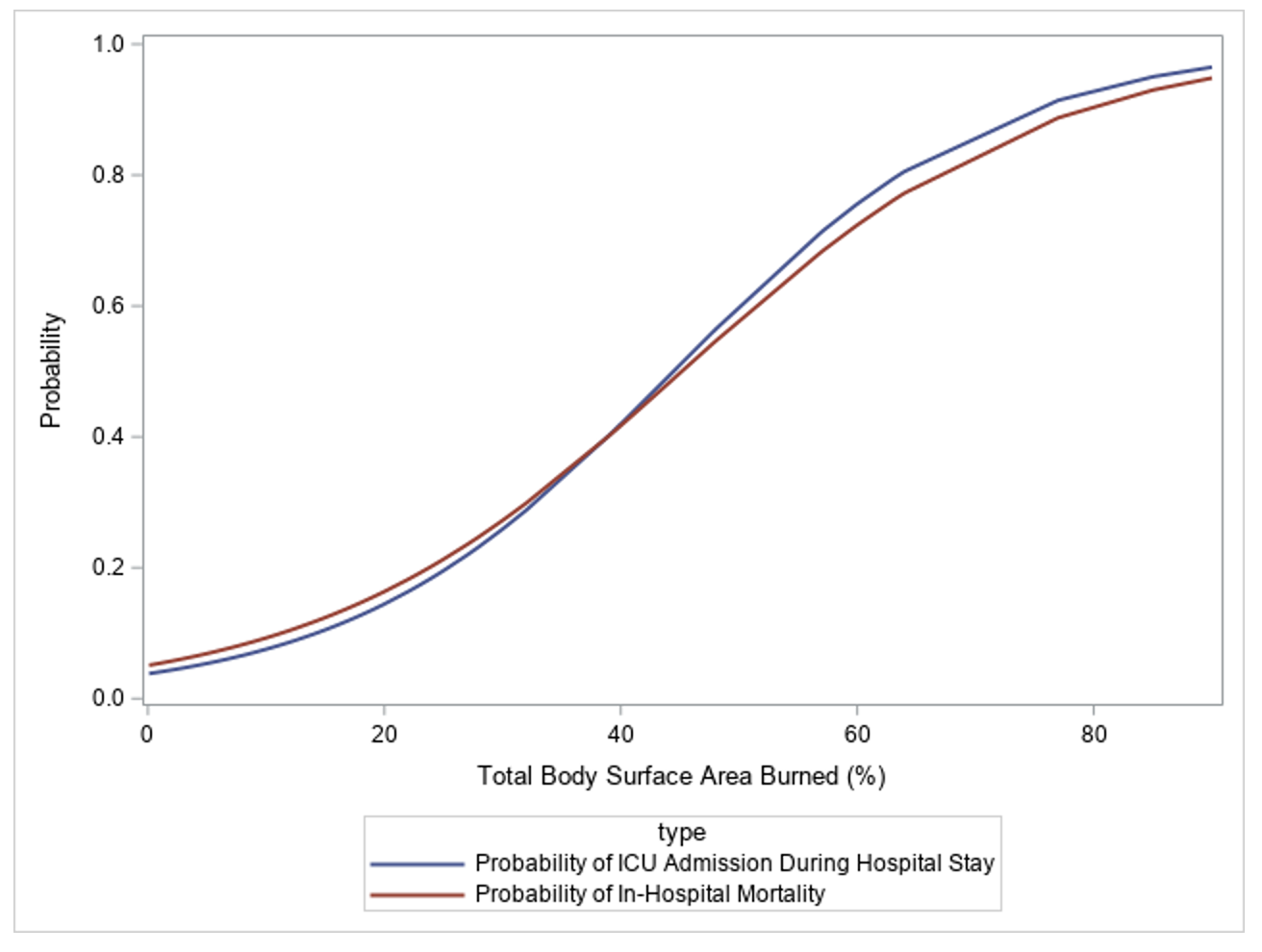
Design/Methods: This was an observational study using data from a pediatric injury registry at Kilimanjaro Christian Medical Center (KCMC). We included patients less than 18 years of age with a burn injury that occurred within 30 days prior to presentation to the KCMC ED. We evaluated morbidity using the previously-validated Glasgow Outcome Scale – Extended for Pediatrics (GOS-E). We tested for differences in burn severity, vital sign abnormalities upon arrival to the ED, and time between injury and arrival to KCMC with ICU admission, morbidity, and in-hospital mortality using t-tests and Fisher’s exact test. We used logit curves to estimate probability of in-hospital mortality and ICU admission by percent total body surface area (TBSA) burned.
Results: We enrolled 99 pediatric burn injury patients from November 2020 to September 2023. The overall mortality rate was 22.2%. When TBSA burned was 50% or greater, the probability of both ICU admission and in-hospital mortality was greater than 50% (Figure 1). Significant factors (p < 0.05) associated with ICU admission and in-hospital mortality included hypothermia and hypoxemia on arrival and intubation in the ED. Hypoxemia and intubation were also significantly associated with higher morbidity (GOS-E score 3-7). In assessing delay to care, median time from injury to KCMC was 20 hours with 25% of patients arriving almost 4 days after their initial injury. Mortality was 33% in patients arriving roughly 4 days after the initial injury compared to 19% in those arriving within 4 days of the initial injury (p=0.16).
Conclusion(s): The in-hospital mortality rate of pediatric burn patients in our cohort was high. Our findings suggest that patients with large burns, delayed ED arrival, or vital sign abnormalities would benefit from escalation of care in the ED. Further evaluation with a larger cohort is needed; however, this data is a starting point in the development of evidence-based pediatric burn care guidelines in Northern Tanzania.