Clinical Bioethics
Session: Clinical Bioethics
425 - Are we saying what we mean to? A qualitative study on how neonatologists offer choices to parents during consultations for extremely preterm deliveries.
Sunday, May 5, 2024
3:30 PM - 6:00 PM ET
Poster Number: 425
Publication Number: 425.1785
Publication Number: 425.1785

Emma N. Prichard, DO (she/her/hers)
Neonatal-Perinatal Fellow
Brooke Army Medical Center
San Antonio, Texas, United States
Presenting Author(s)
Background: As the field of neonatology advances, our ability to care for extremely preterm infants improves but significant risk of morbidity and mortality remains. Shared decision making is recommended for helping parents make plans for delivery room care in these cases. In addition to time constraints and emotional distress, decisions may be negatively affected when parents are not aware a decision is required and by providers introducing biases through framing of choices.
Objective: The aim of this project is to characterize how neonatologists present choices about resuscitation to parents during perinatal counseling for an imminent extremely preterm delivery.
Design/Methods: This project is a qualitative thematic analysis of video recorded mock perinatal counseling sessions between a neonatologist and a simulated patient facing possible delivery at 22 weeks gestation after rupture of membranes. Videos were transcribed and coded for the introduction of a choice about resuscitation. Coding was first performed independently by three individuals of varying backgrounds (neonatology, general pediatrics, and social work) then further refined after meeting as a group. Thematic analysis was then used to inductively derive and examine resulting themes with a fourth researcher.
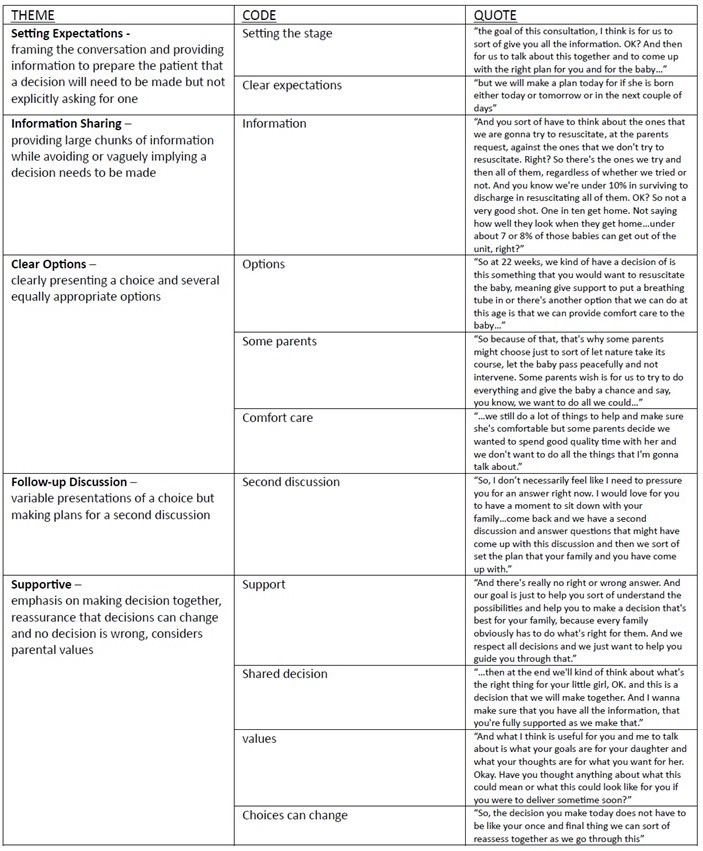
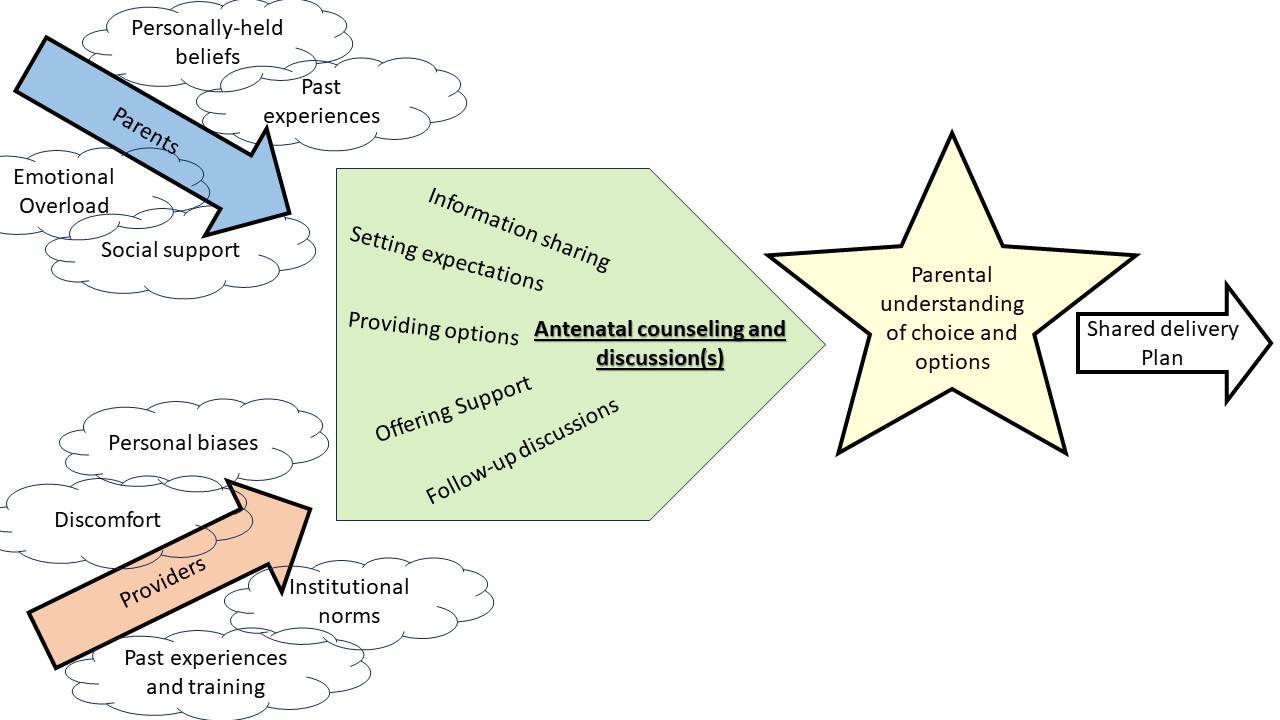
Results: Thematic analysis of the 22 mock consultations revealed five main themes (Table 1): (1) setting expectations – framing the conversation in an attempt to prepare the patient that a decision will need to be made (2) information sharing – providing large chunks of information while avoiding or vaguely implying a decision to be made (3) clear options – clearly presenting a choice and several equally appropriate options (4) follow-up discussion – variable presentations of a choice but making plans for a second discussion (5) supportive – emphasis on making decisions together, importance of parental values and reassurance. These themes were found to interweave throughout the antenatal consult in varying ways but would ideally lead to a shared decision for resuscitation after birth (Figure 1).
Conclusion(s): The neonatologists consulting for possible delivery at 22 weeks in our study had varied approaches that did not always foster shared decision making. The development of best practices and more formalized training in shared decision-making consultation for such deliveries is needed.