Quality Improvement/Patient Safety
Session: Quality Improvement/Patient Safety 3
1 - A process improvement initiative to standardize care coordination for patients requiring nasogastric tube feedings at home
Monday, May 6, 2024
9:30 AM - 11:30 AM ET
Poster Number: 1
Publication Number: 1.3232
Publication Number: 1.3232

Lisa Rickey, MD, MHQS
Pediatric Hospitalist
Boston Children's Hospital
Boston, Massachusetts, United States
Presenting Author(s)
Background: Discharging hospitalized patients with nasogastric tubes (NGT) for enteral nutrition at home is a common, though complex, process. A safe, efficient discharge requires intricate transitional care coordination and education between patients, families, and a multidisciplinary team. In our institution there was no established, standardized pathway to guide providers through the hospital to home transition for this patient population.
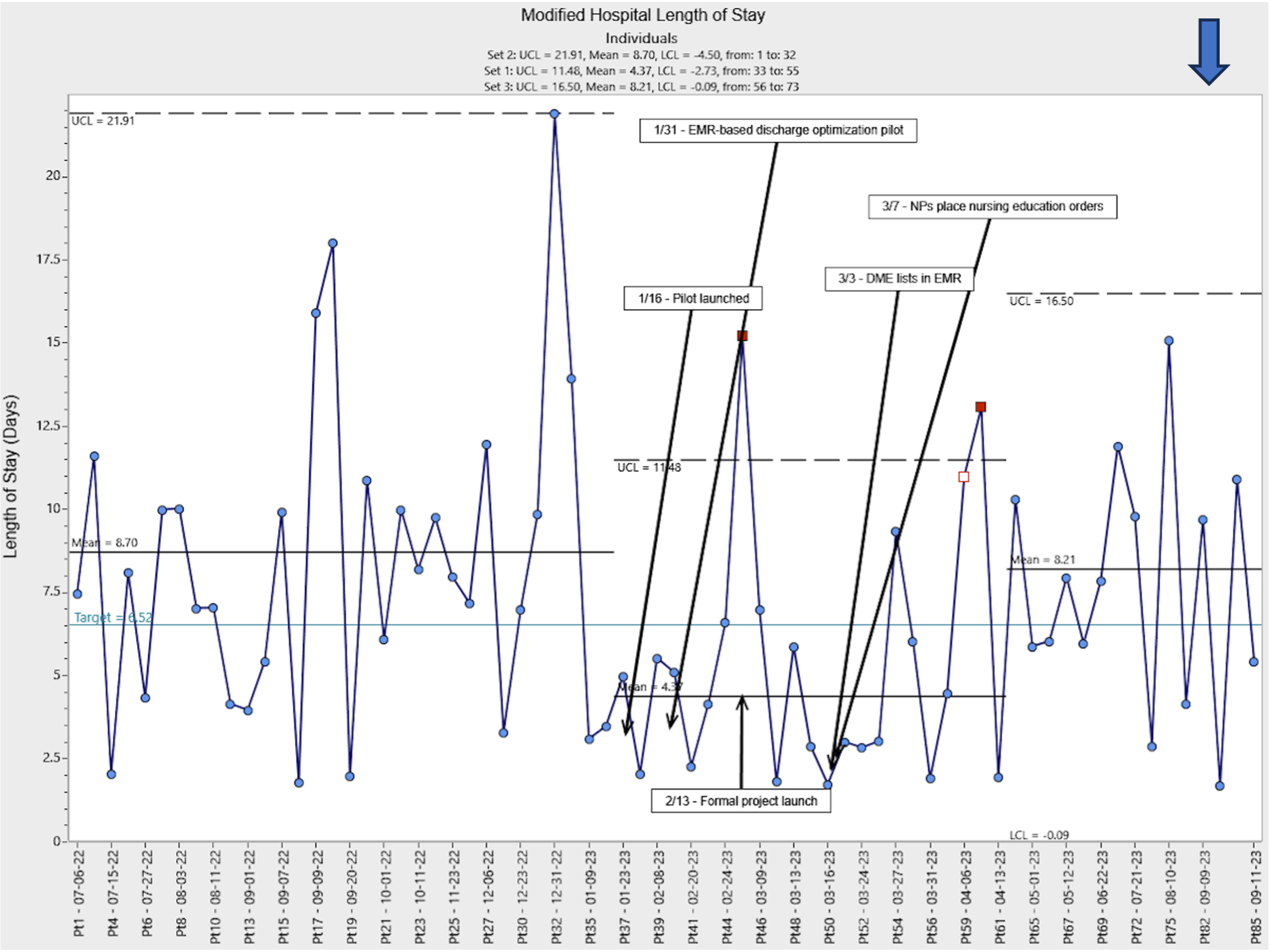
Objective: To (1) reduce variation in and (2) improve the efficiency of transitional care coordination for patients requiring NGT for home enteral nutrition on a pediatric hospital medicine service using standard quality improvement methods. We aimed to reduce the mean modified hospital length of stay (mLOS) by 25% within 3 months.
Design/Methods: A multidisciplinary key stakeholder team created a standardized care algorithm to guide providers through the NGT care coordination process. Key interventions included standardizing providers and role delineation, introducing early and universal consultation of our institution’s Enteral Tube Service (ETS), comprehensive, electronically available lists for home durable medical equipment (DME). We utilized Plan-Do-Study-Act cycles to implement interventions to reduce preventable delays in care, which included removing resident physicians from the care coordination process and creating formula substitution reference documents. Our primary outcome measure was mLOS, defined as time from NGT placement to hospital discharge, which was measured over time in a statistical process control I-chart. Process measures included time from NGT placement to ETS consult. Our balancing measure was 30-day healthcare reutilization.
Results: To date mLOS for included patients has decreased from a baseline of 8.7 days to 8.2 days during the initiative. Early improvements in mLOS were likely tempered because of general patient complexity and acuity. Despite this we have observed narrowing of our control limits to indicate reduced process variability over time. Time from NGT placement to ETS consult has decreased from a mean of 3.9 days to 2.2 days during the intervention period. There were no significant differences in 30-day all-cause healthcare reutilization.
Conclusion(s): This improvement work demonstrates the complexity of inpatient care coordination for enteral nutrition via NGT at home. We have demonstrated reduced variability in process execution over time. Moving forward, local teams plan to scale this pilot intervention across our institution to standardize care and education provided to families who will care for patients with NGTs at home.
.png)