Global Neonatal & Children's Health
Session: Global Neonatal & Children's Health 1
483 - Morbidity and Healthcare Seeking After Hospital Discharge Among Young Children in Dar es Salaam, Tanzania and Monrovia, Liberia
Friday, May 3, 2024
5:15 PM - 7:15 PM ET
Poster Number: 483
Publication Number: 483.152
Publication Number: 483.152

Chris A. Rees, MD, MPH (he/him/his)
Assistant Professor
Emory University School of Medicine
ATLANTA, Georgia, United States
Presenting Author(s)
Background: The post-discharge period is a vulnerable time with an elevated risk of mortality for young children in sub-Saharan Africa. While previous studies have identified risk factors for post-discharge mortality among children in sub-Saharan Africa, little attention has been paid to persistent morbidity and health care use among children during the post-discharge period.
Objective: To compare morbidity and healthcare seeking patterns among children aged < 5 years who died to those who survived at least 60 days after hospital discharge
Design/Methods: We conducted a secondary analysis of a prospective observational cohort of children aged < 5 years discharged from neonatal and pediatric wards of two national referral hospitals in Dar es Salaam, Tanzania (Muhimbili National Hospital) and Monrovia, Liberia (John F. Kennedy Medical Center), 2019-2022. Caregivers of enrolled participants received phone calls up to 60 days after hospital discharge to measure morbidity (i.e., symptoms), healthcare seeking patterns (i.e., hospitalizations, clinic visits, etc.), and vital status. We compared the frequency of reported symptoms and healthcare facility encounters among children who died within 60 days of hospital discharge and those who survived using Chi-square testing.
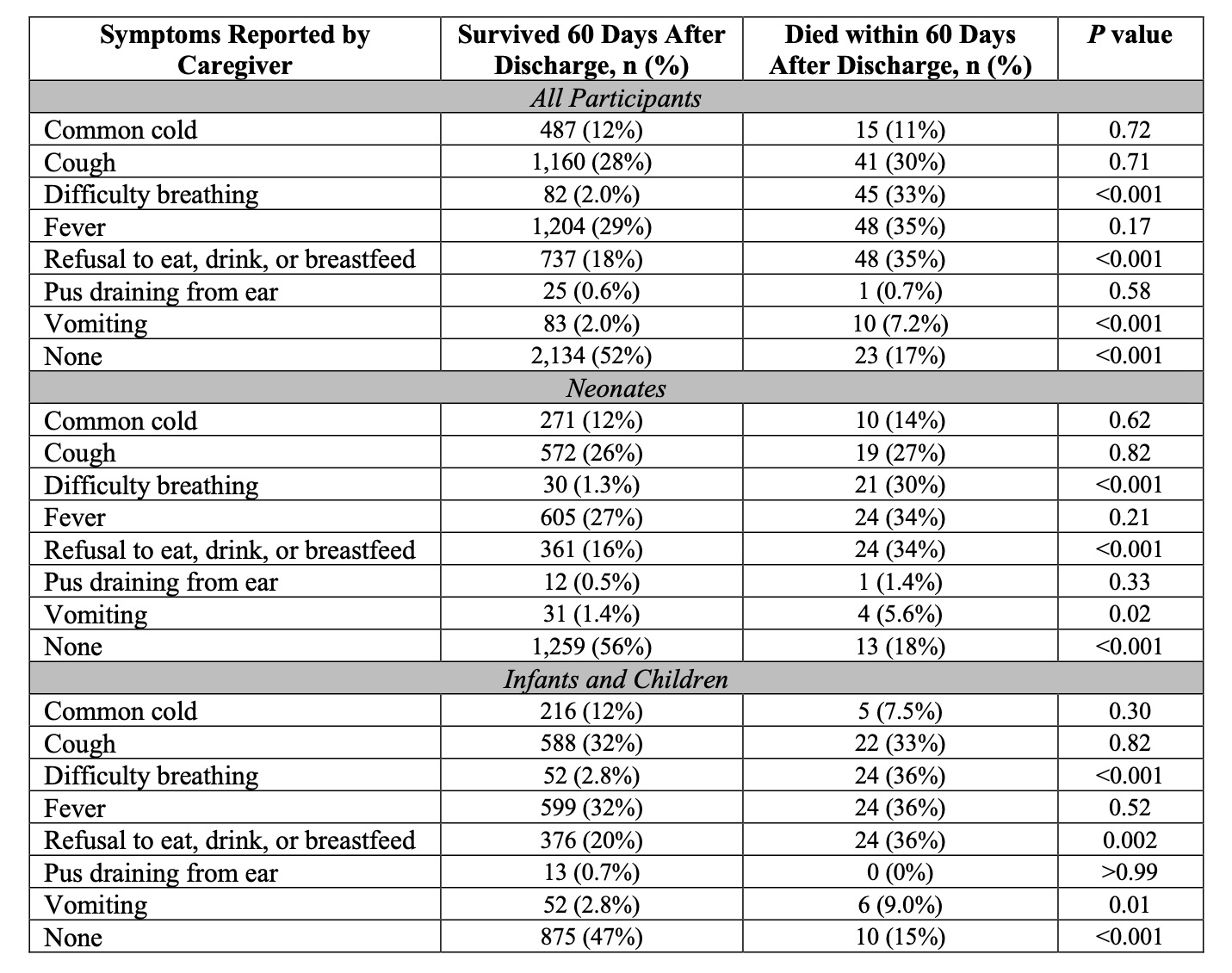
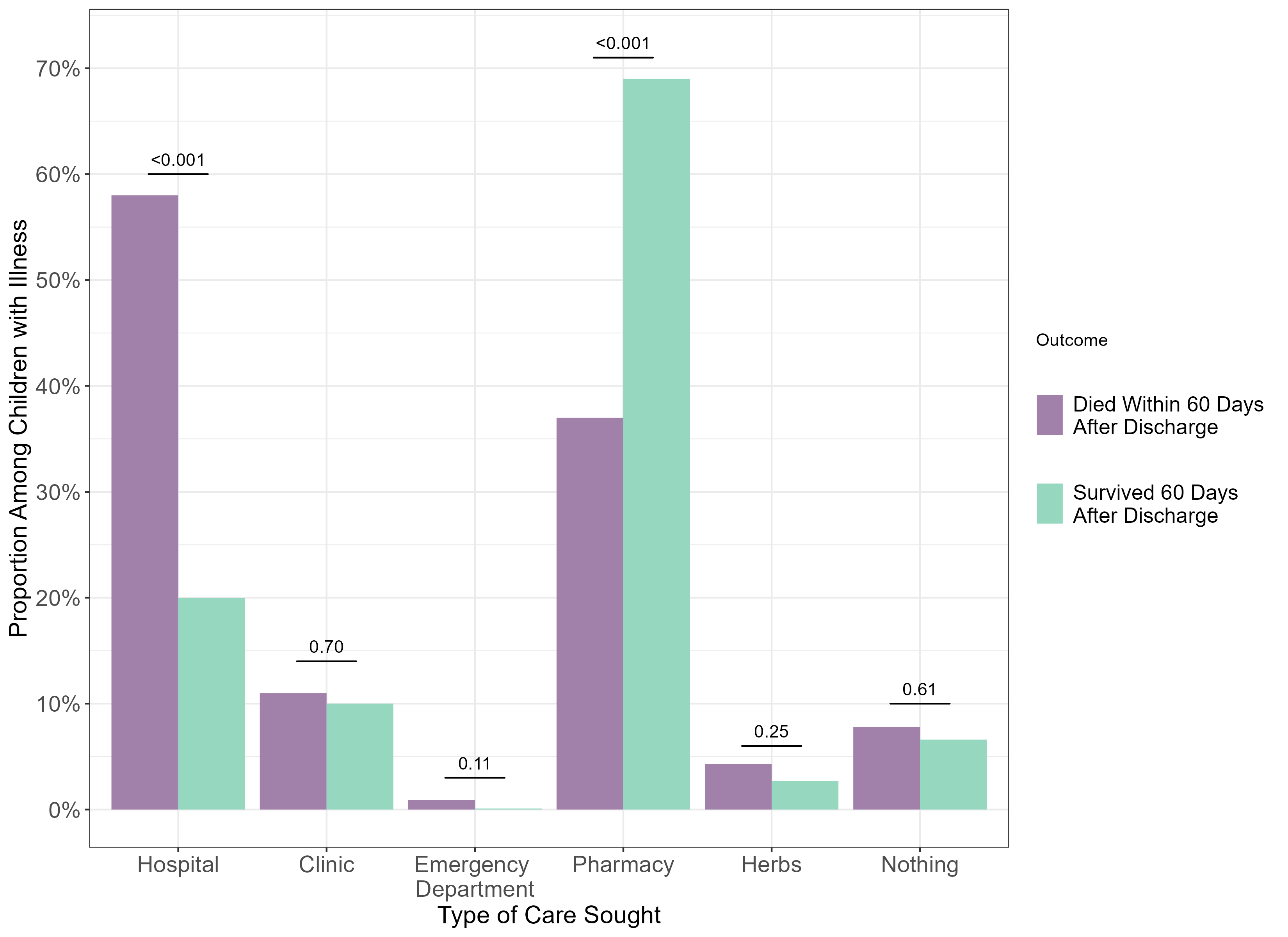
Results: A total of 4,105 participants (96.7%) survived at least 60 days after discharge and 138 (3.3%) children died. The median age of enrolled participants was 1 month (interquartile range [IQR] 0, 9) and 43.8% were female. There was approximately equal enrollment at each site (47.0% in Tanzania and 53.0% in Liberia). Children who died were more likely to have any reported symptom, to have difficulty breathing, refusal to eat/drink/breastfeed, and vomiting following discharge than children who survived with the greatest survival difference noted for children without difficulty breathing (Table). Children who died had a longer median duration of cough after discharge (4 days, IQR 3, 5.5 days) than those who survived (median 3 days, IQR 3, 5 days; P=0.01). Otherwise, we identified no substantial differences in the duration of other symptoms between children who died 60 days after hospital discharge and those who survived. Children who died following hospital discharge were more likely to be readmitted for additional care at a hospital and those who survived were more likely to receive care at a pharmacy (Figure).
Conclusion(s): Targeted surveillance for persistent or new symptoms following hospital discharge is crucial to identify children at risk for post-discharge mortality.