Neonatology
Session: Neonatal Quality Improvement 3
410 - A Qualitative Investigation of Nursing & Caregiver Perspectives on Safe Sleep Education and Implementation in a Level IV Neonatal Intensive Care Unit
Sunday, May 5, 2024
3:30 PM - 6:00 PM ET
Poster Number: 410
Publication Number: 410.1811
Publication Number: 410.1811

Alice Burgess, MD (she/her/hers)
PGY2 Pediatrics Resident
University of Colorado School of Medicine
Denver, Colorado, United States
Presenting Author(s)
Background: 10-15% of U.S. newborns require Neonatal Intensive Care Units (NICUs) admission annually. Preterm and low birth weight infants are 2-3x more likely than term infants to die of sudden unexpected infant death (SUID) and remains the leading cause of death for infants ages 1 month to 1 year. Despite known high risk, NICU providers do not consistently model safe infant sleep. While many infants in the NICU initially require therapeutic positioning due to medical fragility, the American Academy of Pediatrics (AAP) recommends initiation of Safe Sleep when medically eligible. While the pediatric community is aware of this gap in safe sleep modeling and teaching in the NICU, little is known about why this gap persists.
Objective: The objective of this study was to elucidate nursing and caregiver perspectives on the facilitators and barriers to safe sleep education and implementation in a level IV NICU.
Design/Methods: In this phenomenologic qualitative study, current NICU nurses at our institution and caregivers who had an infant admitted to any level IV NICU within the past year were eligible to participate. Semi-structured interviews sought to understand both barriers and supportive factors to modeling and teaching about safe sleep in the NICU. Interview guides focused on perceived obstacles to implementation; teaching methodology and optimal timeline; novel teaching tools; memorable interactions; and infant-specific risk factors. Themes from coded interview transcripts were identified using inductive thematic analysis.
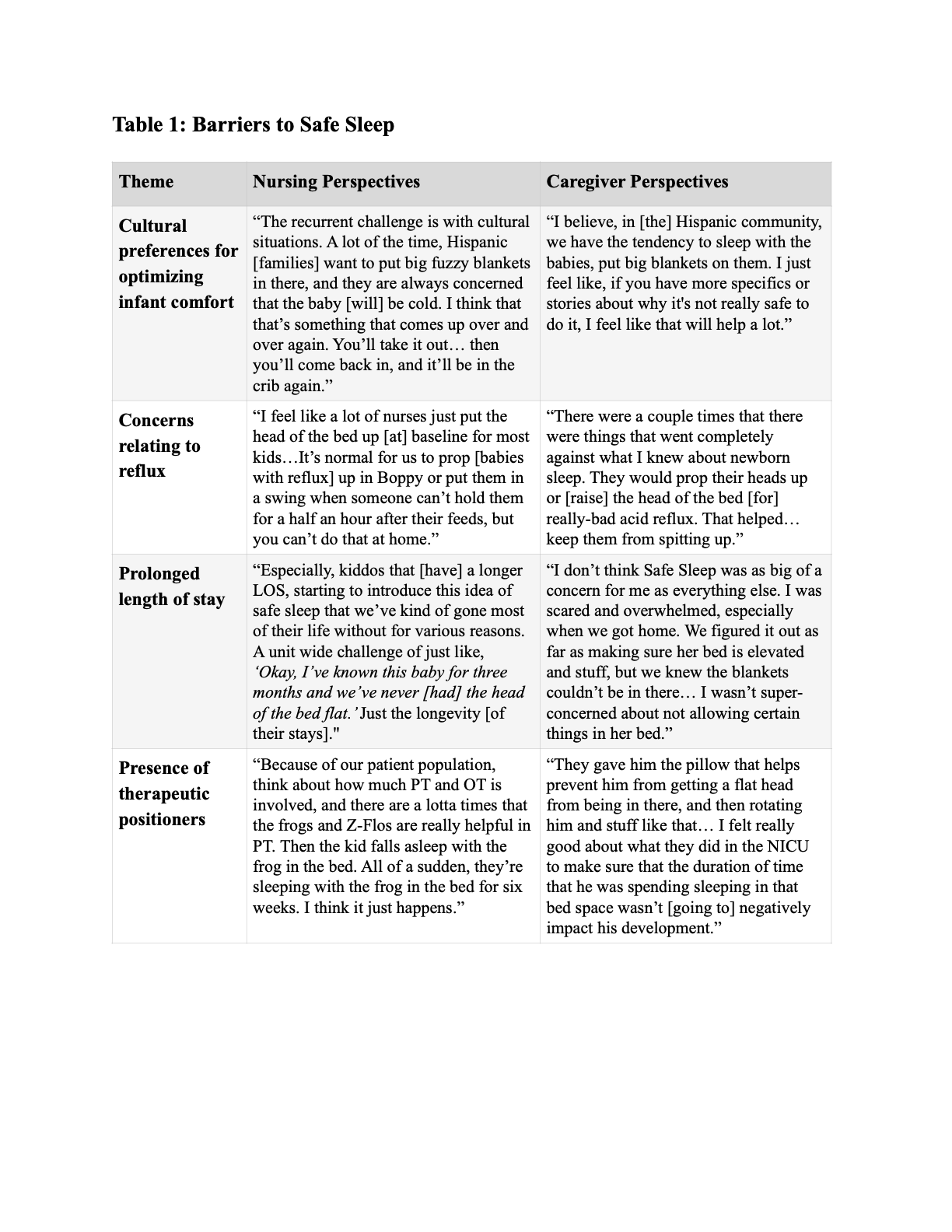
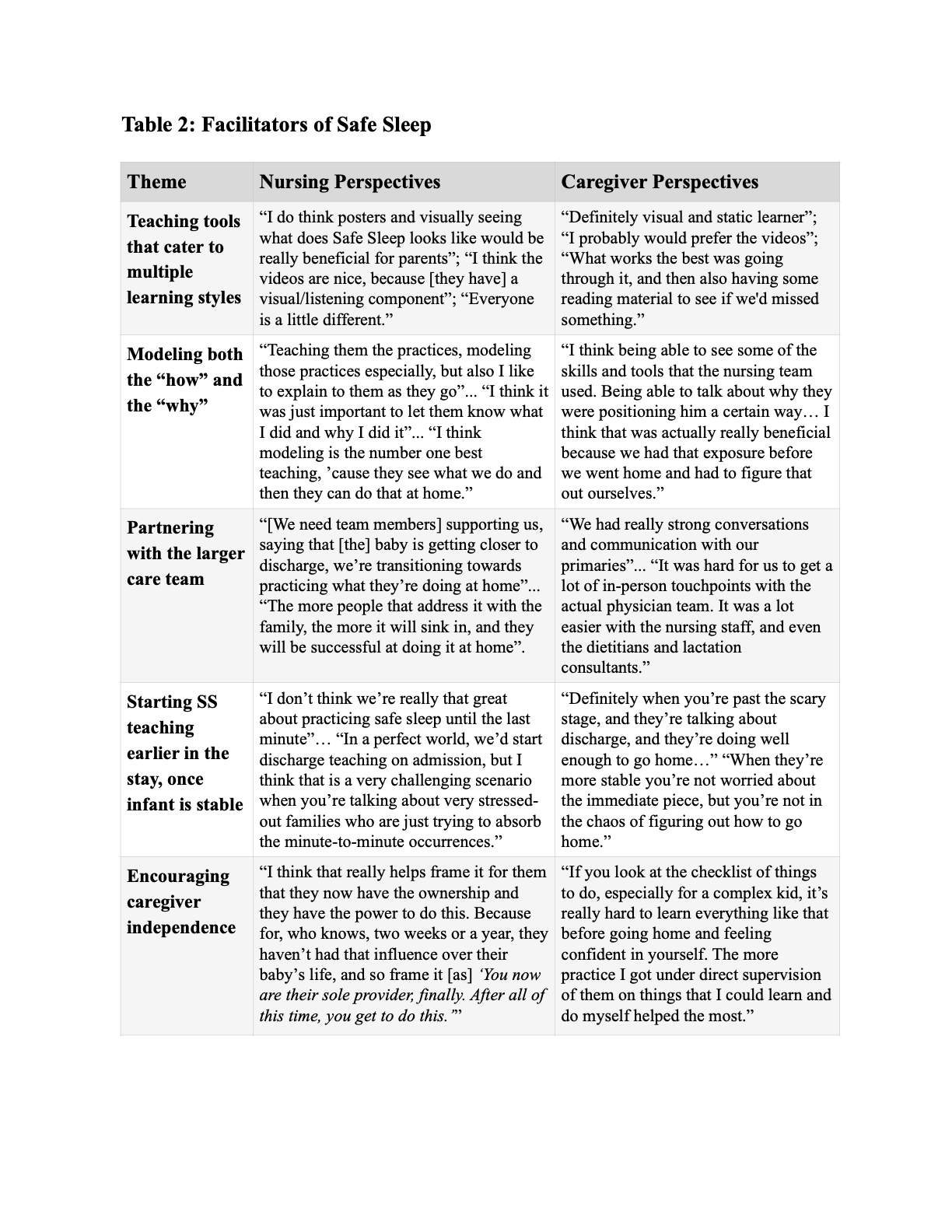
Results: Twenty nursing interviews and ten caregiver interviews were conducted. The mean nursing experience duration was 7.2 years (range of 2 months to 26 years) and included nurses who work both day and night shift. The mean gestational age of infants whose parents participated was 34 weeks (range 27-39 weeks); the average length of stay was 61 days (range of 7-249 days). Themes that emerged included four barriers to safe sleep (cultural preferences; reflux; prolonged length of stay; and therapeutic positioning) and five facilitators of safe sleep (teaching tools, modeling, team consistency, caregiver independence, and earlier initiation of teaching) (Table 1, 2).
Conclusion(s): We identified barriers to effective safe sleep teaching and implementation in the NICU on the provider (nursing) side and the caregiver side. We were able to gain a deeper understanding of patient-, unit-, and system-level supports that will inform a collaborative, equitable, and sustainable future approach to Safe Sleep in a regional level IV NICU.