Palliative Care
Session: Palliative Care
161 - Clinician Word Choice: Discussion of the Fetus in Fetal Cardiology Consultations
Saturday, May 4, 2024
3:30 PM - 6:00 PM ET
Poster Number: 161
Publication Number: 161.1526
Publication Number: 161.1526

Samantha Syme, BA (she/her/hers)
Medical Student
University of Pittsburgh School of Medicine
Pittsburgh, Pennsylvania, United States
Presenting Author(s)
Background: Congenital heart disease (CHD) is the cause of twice as many deaths in children than all types of childhood cancer combined. While fetal echocardiography has increased prenatal detection of CHD, there is still no framework for how to refer to a fetus when discussing congenital heart disease prenatally. In other prenatal settings, particularly with high fetal mortality risk, families prefer the term, “baby.” In the medical community, there is no consensus on what terminology should be used when discussing the fetus; the term “fetus” is used here as medical terminology in lieu of an agreed-upon word.
Objective: We aimed to identify how clinicians referred to the fetus in initial fetal cardiology consultations.
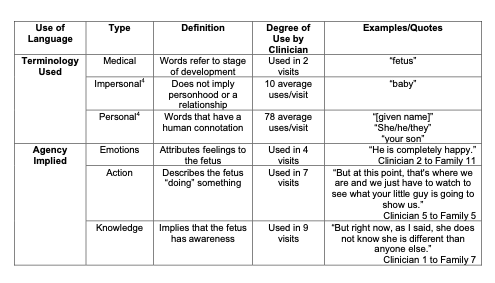
Design/Methods: Initial fetal cardiology consultations were recorded and transcribed verbatim. Any reference to the fetus was coded for this analysis. Codes included noting specific semantics (e.g., “fetus,” “baby”), use of pronouns or names, and any reference to relationship (e.g., “your”). Codes were then examined and categorized. We then noted frequencies of use of specific categories per utterance for each of the recorded visits.
Results: Nineteen consultations were conducted by five clinicians at one academic institution. Clinicians used the following terminology to reference the fetus in decreasing frequency: personal, impersonal, and medical (Table 1). Among the categories, personal was the most commonly used. Most clinicians also implied fetal agency by discussing the fetus having knowledge or emotions or doing an action (Table 1). Personal and impersonal language implied that the fetus was a person by frequently referring to the fetus as a subject rather than an object (e.g., “Is she going to be an artist? Is she going to be a dancer?”) . The use of terminology for the fetus did not differ by mortality risk. Families were not asked for their preferred terminology in any of the appointments.
Conclusion(s): Clinicians implied that the fetus was a person through the terminology used and the agency implied. Future studies should focus on how to assess families’ views of fetal personhood to better align clinicians’ language with families’ beliefs. Families may view personhood as slowly progressing over pregnancy so it is also imperative to investigate how best clinician language can reflect that evolution.