Medical Education
Session: Medical Education 8
492 - Examining and Improving Pediatric Residents’ Understanding of Lactation Medicine through Expert-led Didactic and Clinical Trainings
Monday, May 6, 2024
9:30 AM - 11:30 AM ET
Poster Number: 492
Publication Number: 492.3199
Publication Number: 492.3199

Shanice R. Wells, MD (she/her/hers)
Resident
Sidney Kimmel Medical College at Thomas Jefferson University
Philadelphia, Pennsylvania, United States
Presenting Author(s)
Background: Developing a pediatric work force that is competent to provide families with lactation support within the healthcare system is important to improving lactation rates, yet there is no formalized approach. Only 25% of infants receive human milk through 6 months of life. Pediatricians are positioned to support families with lactation concerns, but despite the vital role that they can have, many pediatricians lack the knowledge and skills to support parent-infant dyads. There is limited existing literature on pediatric trainees’ attitudes towards lactation medicine and how to effectively include this training in residency programs.
Objective: · Design and implement a curriculum for pediatric residents to develop practical skills in assessing and managing human milk fed dyads
· After completion of the curriculum residents will have improved knowledge of lactation medicine and improved self confidence in providing care to lactating dyads
Design/Methods: · Created an outline of the most relevant lactation medicine knowledge and skills for pediatric residents
· Curriculum administered during 2022-23 academic year via lectures, small group discussion and direct work with a lactation consultant
· Administered the AAP Breastfeeding Curriculum pretest (n=17) in July 2022 and the posttest in June 2023 (n = 20) out of a cohort of 28 residents (PGY1, PGY2, PGY3)
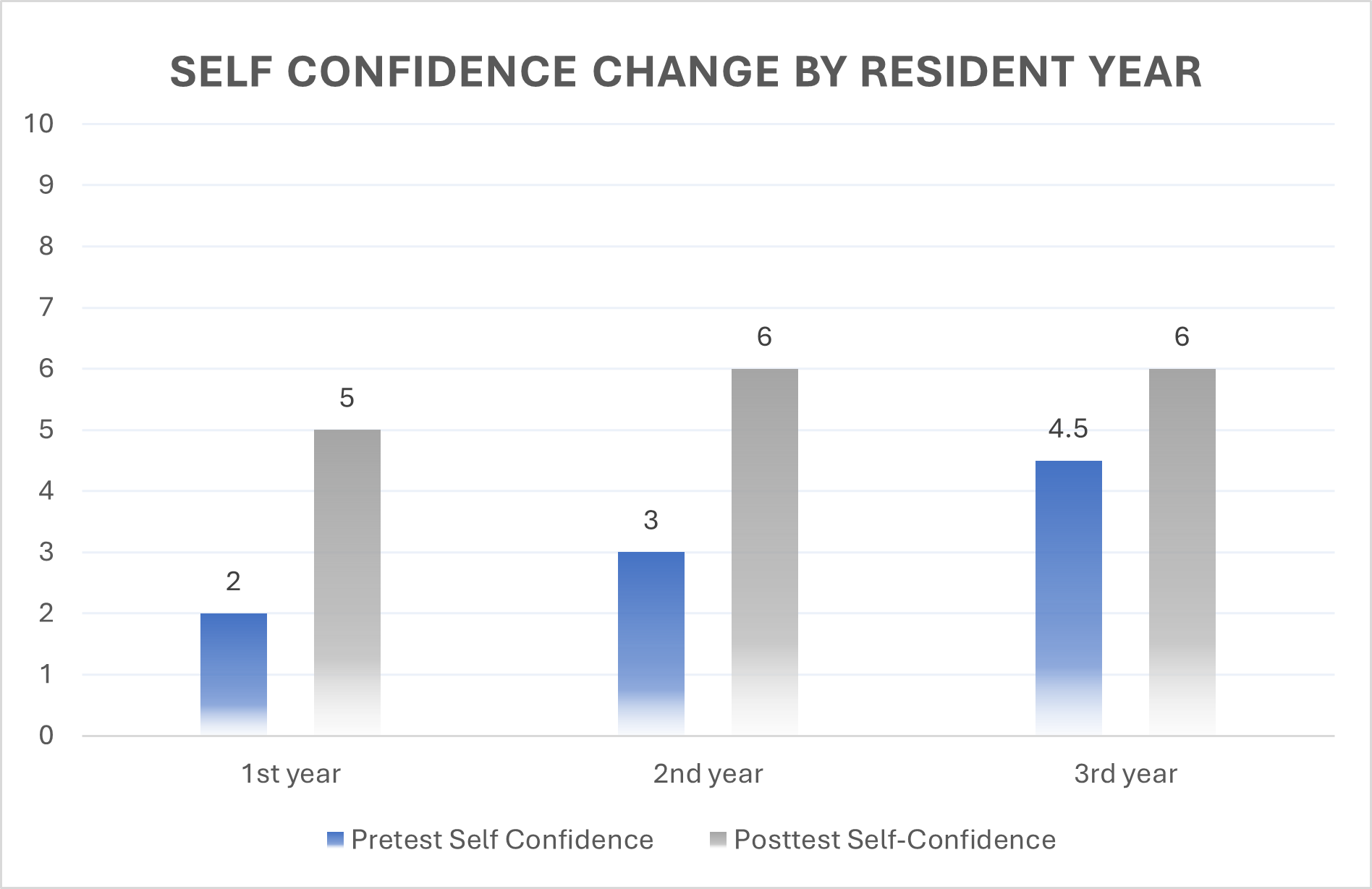
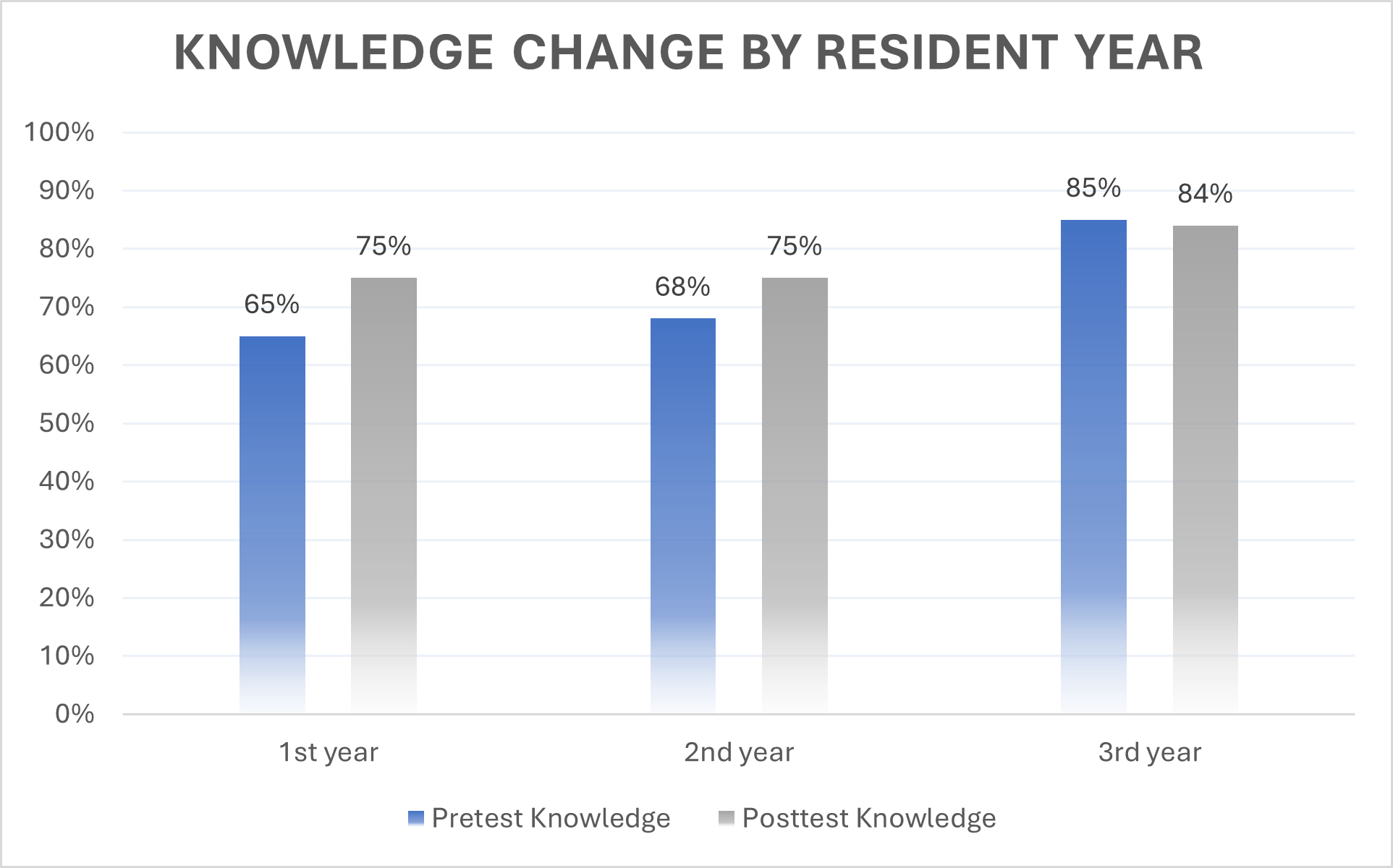
Results: Though all residents participated in the curriculum, not all took both pretest and posttest, so all comparisons are unpaired. Welch two sample t-tests showed significant improvements in knowledge scores from pretest to posttest (69% vs 78%, p = .031). Mann Whitney U test also showed significant improvement in self-confidence scores (out of 10) from pretest to posttest (Median = 3 vs 6, p = .001). Significant positive correlations were found among all pretest scores and resident year, and between training amounts and self-confidence levels post intervention. Two-way ANOVAs revealed only 1st year residents experienced significant increases in knowledge and self-confidence.
Conclusion(s): A standardized curriculum improves knowledge and self-confidence in lactation medicine when taught by an expert through hands-on skills and lectures. There was no increase in the second and third years of residency in knowledge or confidence highlighting the need for continued advanced teaching in this area through a longitudinal lactation curriculum.