Medical Education
Session: Medical Education 2
536 - Point-of-Care Ultrasound (POCUS) Workshop for Pediatric Emergency Medicine Fellows: Pre/Post-Training Assessment of Knowledge and Confidence
Friday, May 3, 2024
5:15 PM - 7:15 PM ET
Poster Number: 536
Publication Number: 536.184
Publication Number: 536.184

Julia A. Ciurria, MB BCh (she/her/hers)
Assistant Professor of Pediatrics, Division of Emergency Medicine
Washington University in St. Louis School of Medicine
St. Louis, Missouri, United States
Presenting Author(s)
Background: Point-of-care ultrasound (POCUS) is a well-established clinical tool in emergency medicine with rapidly increasing integration into other disciplines, such as Pediatric Emergency Medicine (PEM) . Despite increasing demand for POCUS education for PEM trainees, significant variation in training modalities exists across PEM fellowship programs . To better understand the effectiveness of POCUS educational interventions, we surveyed PEM fellows who participated in our institution’s annual POCUS training course.
Objective: This study aims to assess whether a 4-hour training course improved the knowledge and confidence of PEM fellows in using POCUS.
Design/Methods: PEM fellows from 8 different academic institutions participated in this annual 4-hour POCUS workshop over a 4-year period (2020 to 2023). The course consisted of 1.5 hours of didactics and 2.5 hours of hands-on practice with live models and phantoms for procedural skills.
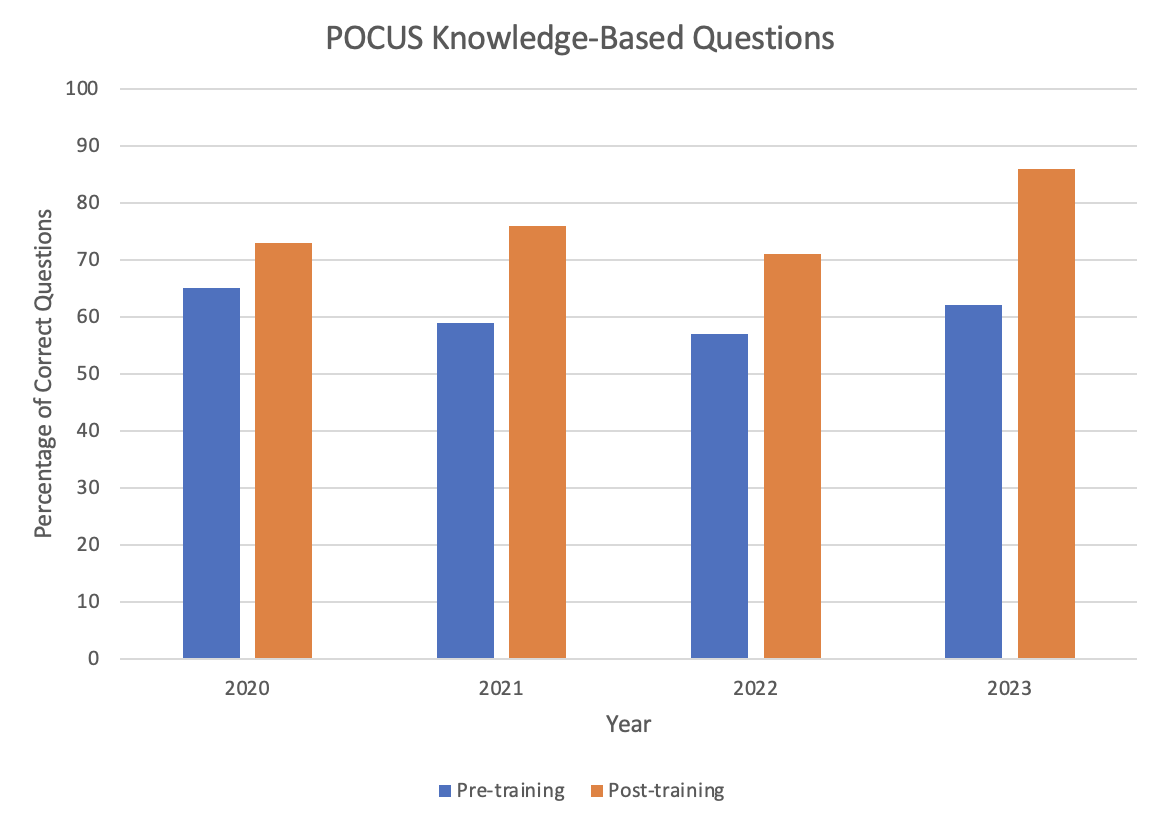
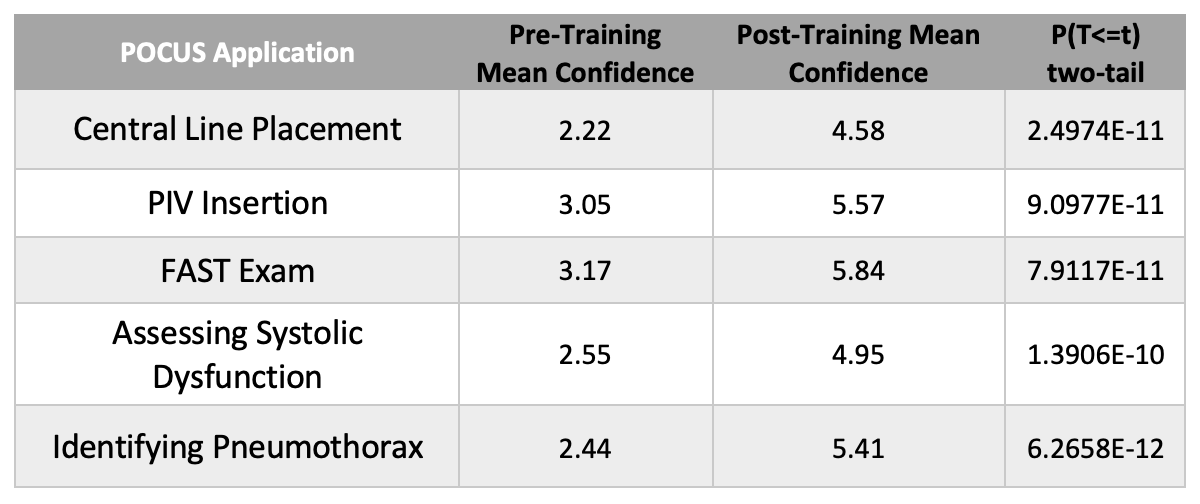
Participants were asked to complete pre- and post-training surveys. 5 identical knowledge-based questions were included. Confidence in POCUS applications was assessed using a 10-point Likert scale (1 representing no confidence and 10 representing complete confidence). At the end of the 4-hour workshop, participants completed a post-training survey to assess improvement in knowledge and confidence.
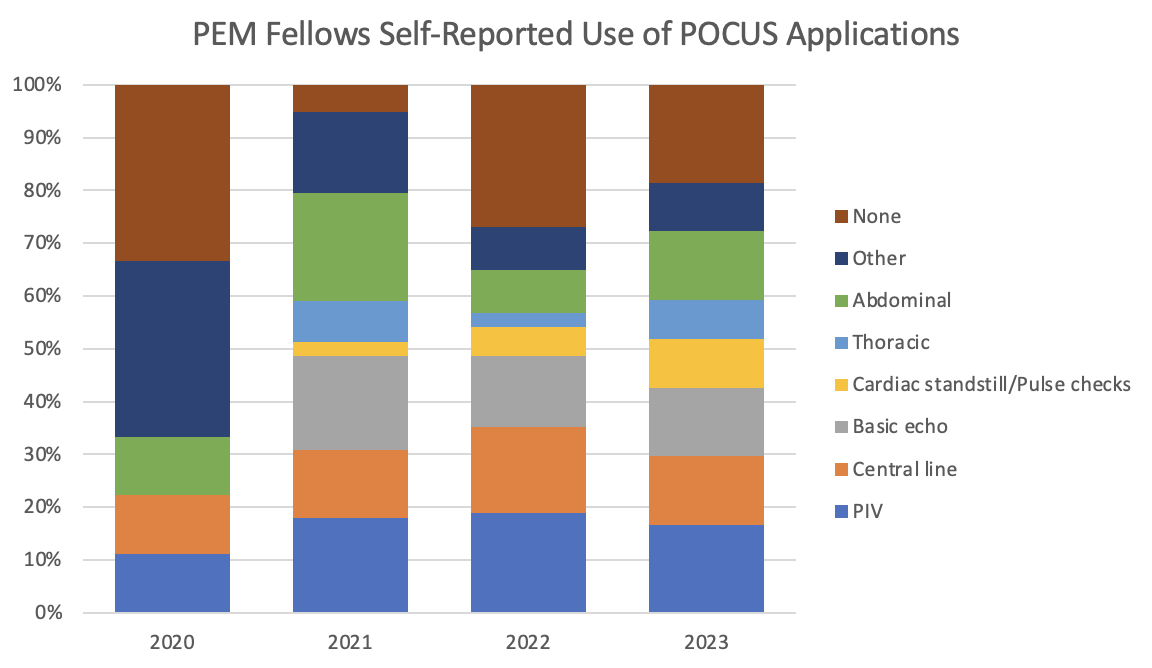
Results: 65 PEM fellows completed the pre-training survey: 64 completed pediatric residency, while 1 was emergency medicine trained. 89% of participants reported no prior POCUS education at any point in their training. Almost 65% of PEM fellows had never used POCUS, while 32% had sometimes used POCUS. The only respondent to report frequent POCUS use was emergency medicine trained. The most commonly used POCUS application was peripheral intravenous catheter (PIV) insertion. PEM fellows had the highest pre-training confidence with focused assessment with sonography for trauma (FAST) scans.
64 PEM fellows completed the post-training survey. The highest post-training confidence was reported with FAST scans. The greatest self-reported improvement in confidence was with identifying pneumothoraxes. Only 3% of participants reported comfort with current POCUS skill level on the pre-training survey; this improved to 45% on post-training surveys. 100% of participants stated that POCUS is a useful tool for clinical practice in the pediatric emergency department.
Conclusion(s): Through a combination of didactics and hands-on practice, this 4-hour POCUS workshop improved PEM fellows’ knowledge and self-reported confidence with POCUS. Future studies should focus on skill retention over time.