Emergency Medicine
Session: Emergency Medicine 10: Trauma
394 - Disparities in healthcare utilization and functional outcomes of children with cervical spine injury
Monday, May 6, 2024
9:30 AM - 11:30 AM ET
Poster Number: 394
Publication Number: 394.3181
Publication Number: 394.3181
- JW
Jordee M. Wells, MD, MPH (she/her/hers)
Assistant Professor of Pediatrics
Nationwide Children's Hospital
Columbus, Ohio, United States
Presenting Author(s)
Background: The evidence for health disparities within pediatric trauma is growing, however there is little information regarding children with cervical spine injuries (CSIs).
Objective: To evaluate disparities in healthcare utilization and functional outcomes for children with CSI.
Design/Methods: This was a planned mixed methods study that included secondary analysis of a multi-center, prospective study of children 0-17 years with blunt trauma evaluated at 18 Pediatric Emergency Care Applied Research Network emergency departments and semi-structured interviews of caregivers of non-deceased children with CSIs, which occurred between 6 and 24 months after diagnosis. Social factors were assessed with the Protocol for Responding to and Assessing Patient’s Assets, Risks, and Experiences (PRAPARE). Healthcare utilization was assessed based on healthcare services received in the cognitive, physical, socioemotional, functional, and health-related social needs domains by standardized responses adapted from National Health Interview Survey (NHIS). Unmet healthcare need was a composite measure defined by the report of social needs in PRAPARE and/or report of healthcare services need in NHIS. Functional outcomes were assessed with the NIH Common Fund’s Patient-Reported Outcomes Measurement Instrument System (PROMIS) tool. Differences in participant characteristics and outcomes were assessed using standard non-parametric methods and multivariable logistic regression.
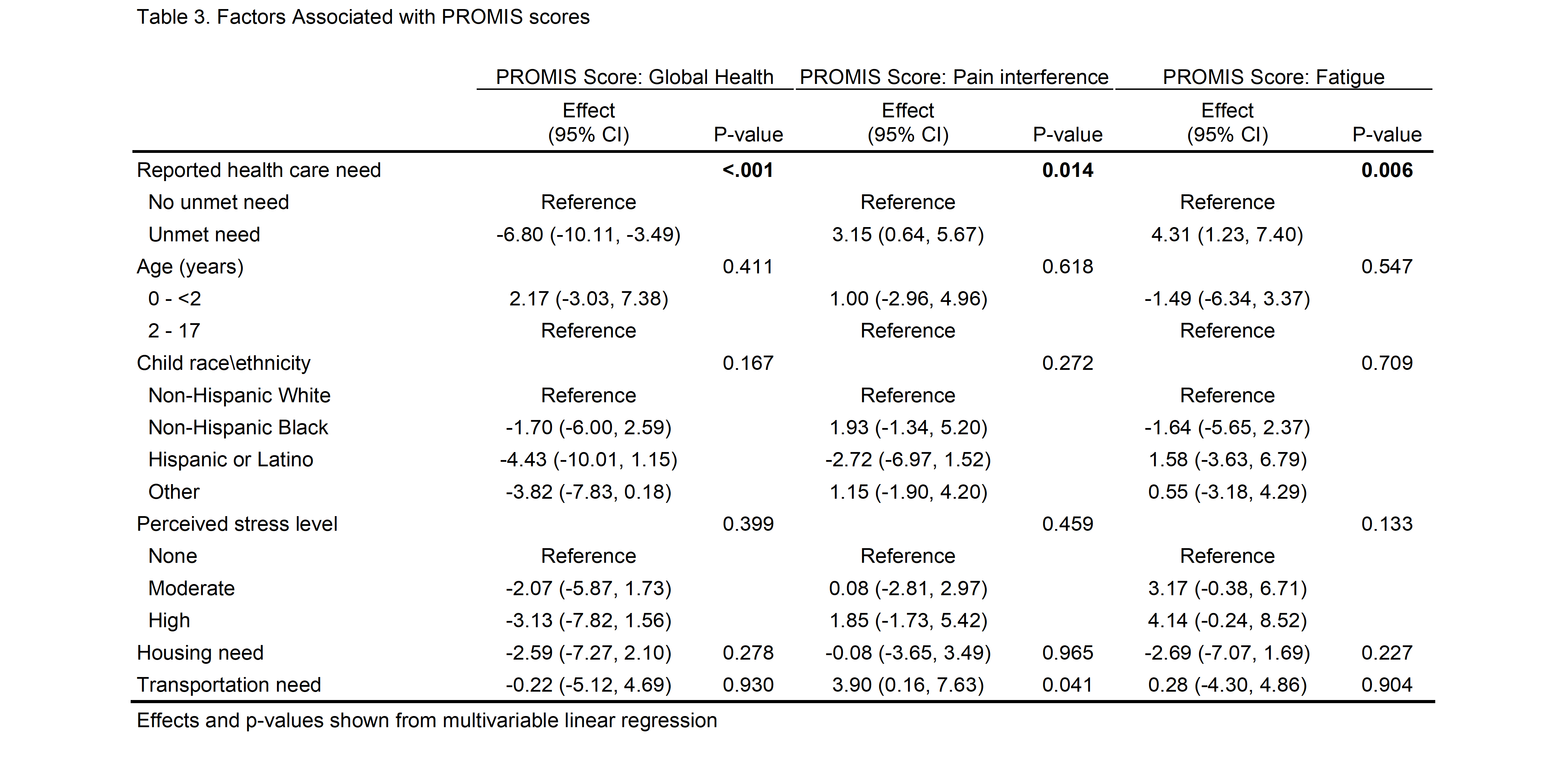
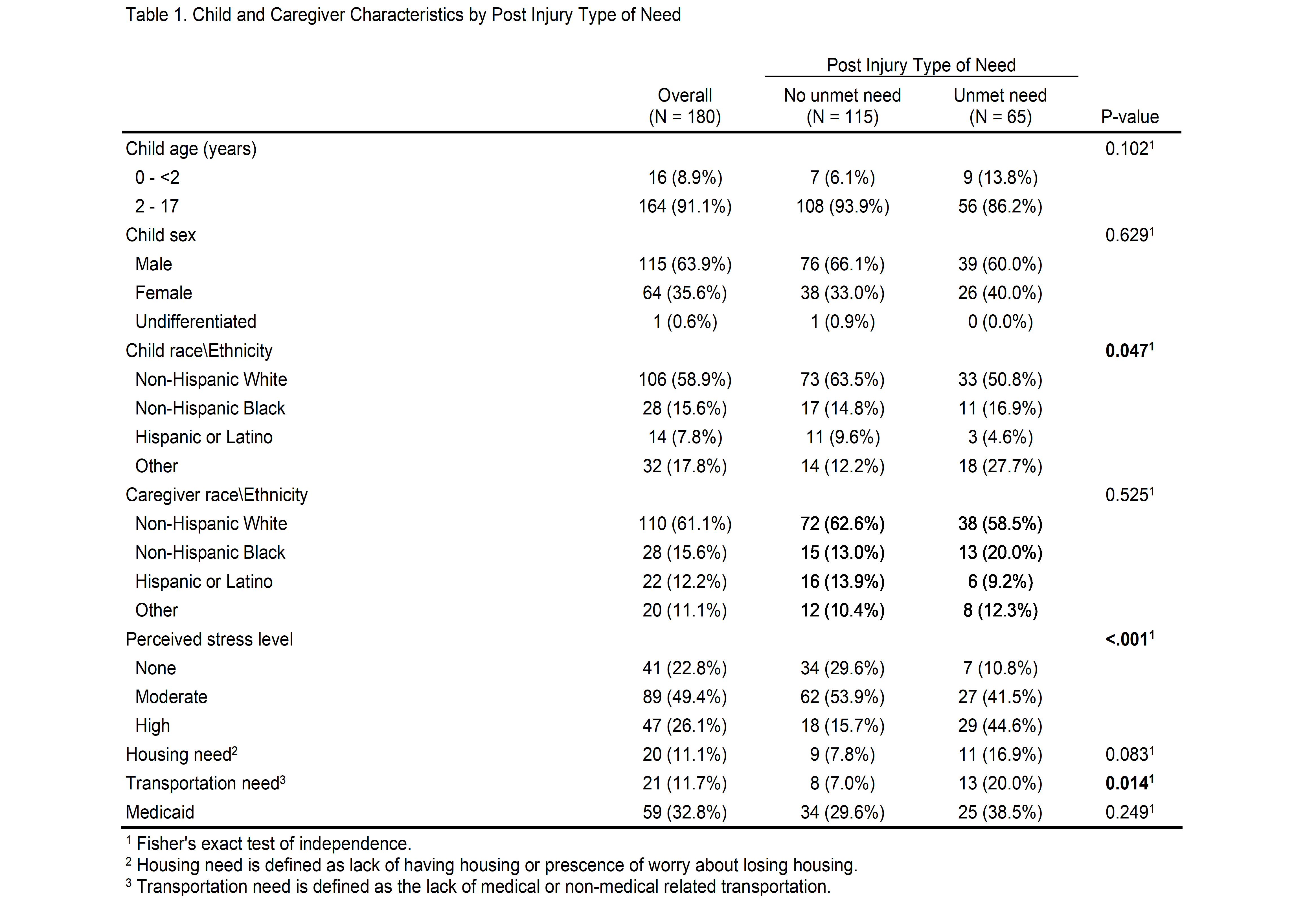
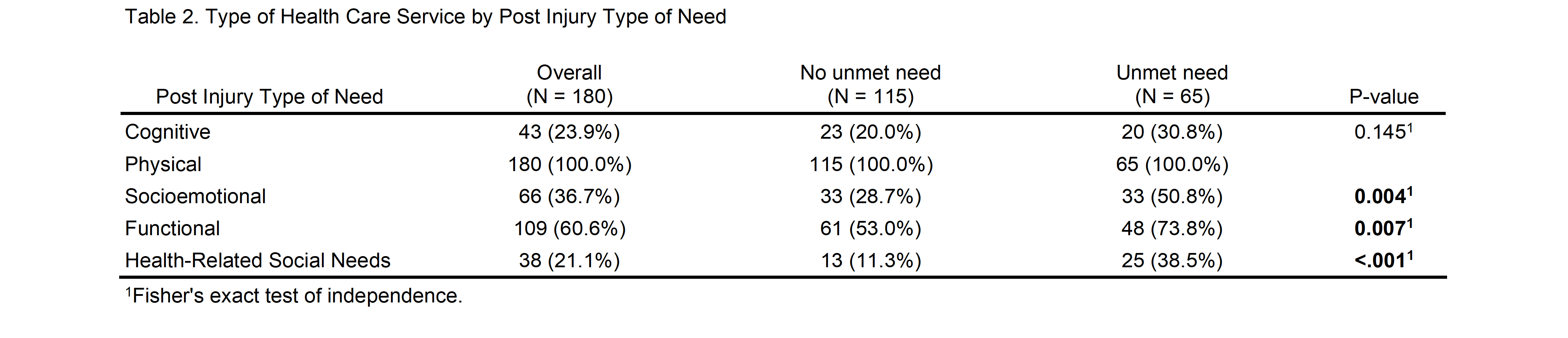
Results: Of the 433 children with CSI, 395 families were approached, and 180 (46%) completed telephone follow up. The report of unmet healthcare needs significantly differed by child race and ethnicity, caregiver perceived stress, and transportation needs [Table 1]. For healthcare utilization, unmet healthcare needs differed between socioemotional, functional, and health-related social needs domains compared to cognitive and physical [Table 2]. For functional outcome, reports of unmet healthcare needs were significantly associated with worse PROMIS outcome scores for global health, pain, and fatigue in multivariable analyses, after controlling for child age and race/ethnicity, provider level of stress, housing need, and transportation need [Table 3].
Conclusion(s): In children with CSIs, racial and ethnic differences exist in healthcare utilization. Caregivers reporting unmet healthcare needs, also reported higher perceived stress and transportation disparities. Unmet healthcare needs were associated with poorer PROMIS functional outcome scores. Future efforts should provide focused support for injured children at higher risk of unmet healthcare needs.