Infectious Diseases
Session: Infectious Diseases 3
127 - Impact of Myeloid Derived Suppressor Cells (MDSC) on T cell Function in Children with Staphylococcus aureus (SA) Infections
Sunday, May 5, 2024
3:30 PM - 6:00 PM ET
Poster Number: 127
Publication Number: 127.1837
Publication Number: 127.1837

Jordan Brauner, MD (she/her/hers)
Fellow
Nationwide Children's Hospital
Columbus, Ohio, United States
Presenting Author(s)
Background: SA causes more than 100,000 pediatric hospitalizations per year. Infections can be severe, including sepsis, pneumonia, or osteoarticular. Children with SA infection demonstrate impaired T cell function. MDSC are immature myeloid cells that potently suppress T cell function via a variety of mechanisms, including binding of programmed death-ligand 1 (PD-L1) to its receptor PD-1 on T cells. MDSC are known to suppress T cells in SA murine models, however, MDSC effects and mechanisms in SA-infected children are unknown.
Objective: We hypothesize that MDSC are expanded in children with SA infection and contribute to T cell impairment.
Design/Methods: We conducted a prospective, observational study in children admitted to the hospital with culture-confirmed SA infection. Age-matched healthy children (HC) without systemic disease or recent infection undergoing minor procedures were enrolled as controls. Peripheral blood mononuclear cells were isolated and stained to identify MDSC (CD45+, HLA-DR-, CD33+, CD11b+), granulocytic (G)-MDSC (CD15+) and monocytic (M)-MDSC (CD14+) subsets, and T cell populations (CD4+, CD8+). Interferon (IFN)γ-secreting T cells were quantified by ELISpot following stimulation with PMA/ionomycin.
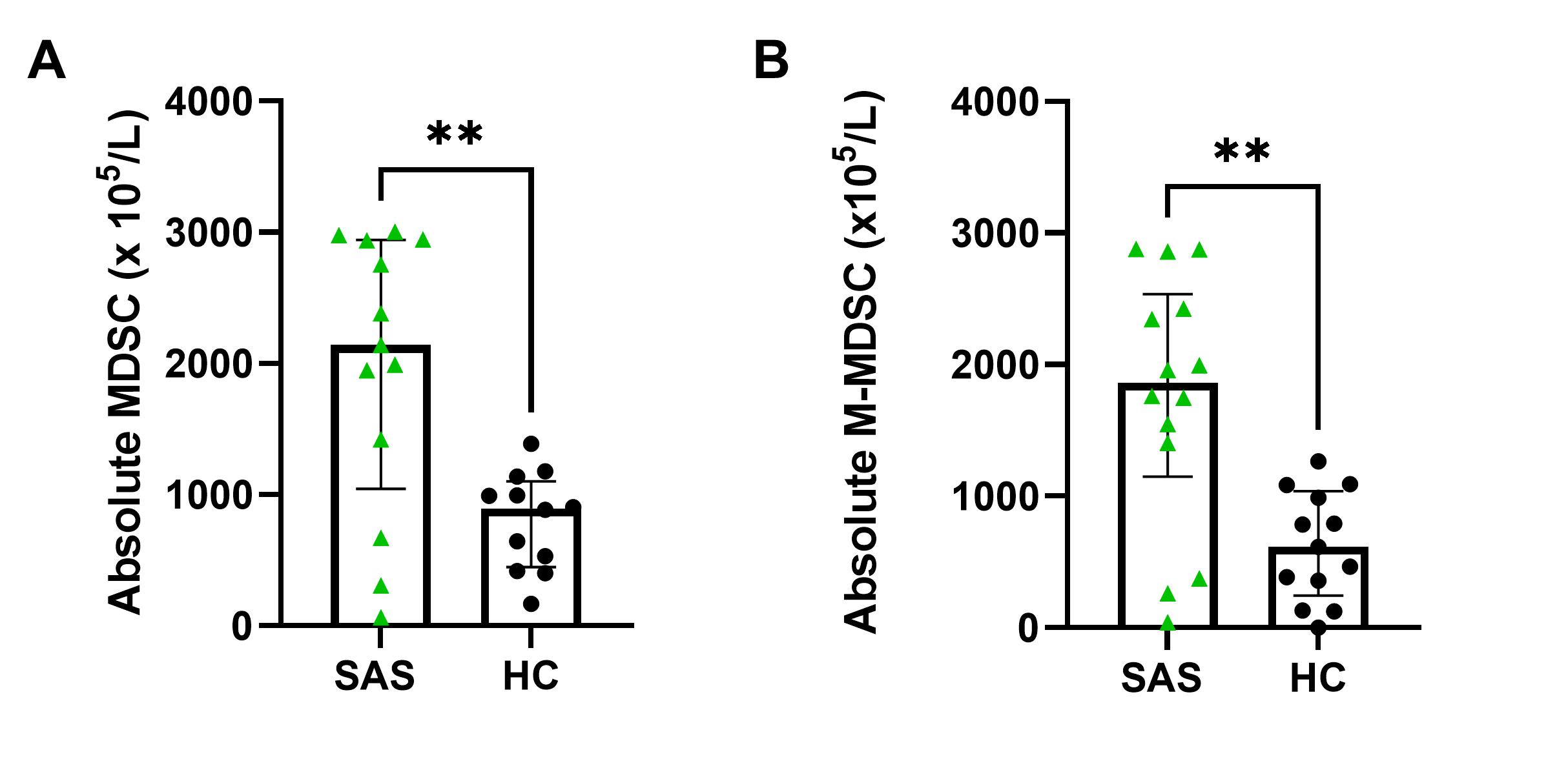
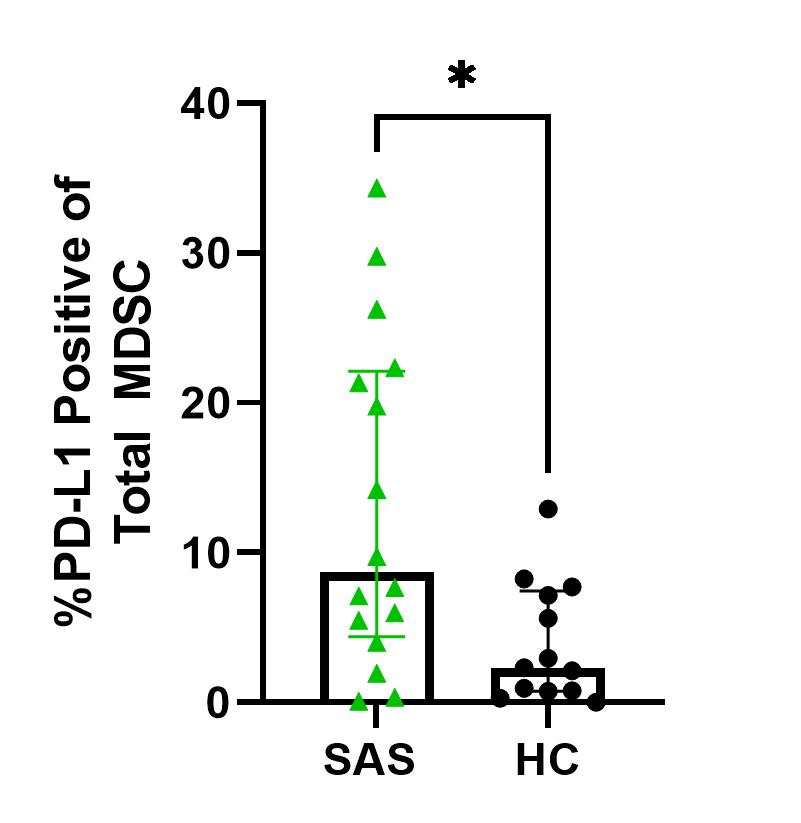
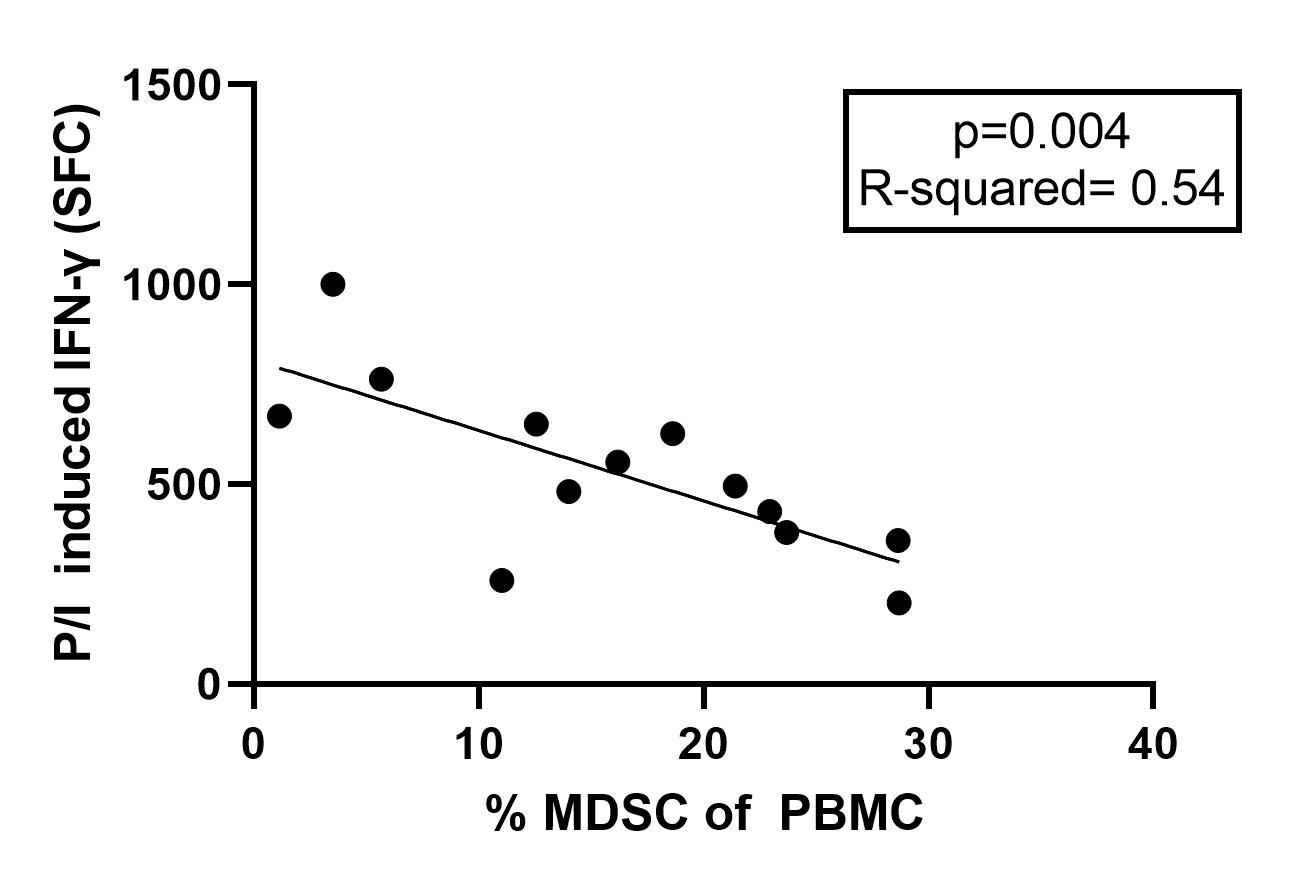
Results: 17 SA infected subjects (SAS) (71% male, median age 10.7 [1.8-18] yrs) and 13 HC (82% male, median age 9 [5.2-17] yrs, p=0.8) were enrolled. SAS had more MDSC compared to HC (median 2143 [66.38-3005] v 895 [167-1388] p=0.008), with M-MDSC predominance (1861 [1149, 2534] v 615 [244,1037], p=0.003) (Fig 1). CD4+ and CD8+ T cell percentages were similar between SAS and HC (CD4+ 59% [36-72] v 60% [43-66] p=0.7, CD8+ 24% [14-40] v 28% [23-41] p=0.2). SAS also demonstrated significantly higher expression of PD-L1 compared to HC (8.7% [4.4-22] v 2.3% [0.8-7.4], p=0.03) (Fig 2). IFNγ secreting T cells were decreased in SAS compared to HC (499 [251-696] v 1000 [554-1000] p< 0.0001). Linear regression analysis demonstrated increased percentage of MDSC was associated with decreased IFNγ secreting T cells in SAS. (R2=0.54, p=0.004) (Fig 3).
Conclusion(s): Our results show that MDSC, particularly M-MDSC, are expanded in SAS and have higher expression of PD-L1 compared to HC. Additionally, SAS have similar percentages of T cells but significantly decreased T cell IFNγ production compared to HC. These data suggest that MDSC expansion impairs T cell cytokine production via increased expression of PD-L1. Further studies are needed to confirm the PD-1 pathway as a potential therapeutic target to inhibit MDSC-mediated T cell suppression in children with SA infection and improve outcomes.