Global Neonatal & Children's Health
Session: Global Neonatal & Children's Health 1
482 - Maternal risk factors and growth of low-birth weight infants in rural Sierra Leone
Friday, May 3, 2024
5:15 PM - 7:15 PM ET
Poster Number: 482
Publication Number: 482.195
Publication Number: 482.195

David Hendrixson, MD (he/him/his)
Assistant Professor
University of Washington School of Medicine
Seattle, Washington, United States
Presenting Author(s)
Background: Millions of infants are born low birth weight (LBW) each year with the highest prevalence in low- and middle-income settings. LBW infants are at increased risk of morbidity and mortality compared to non-LBW peers. Identifying contributing maternal factors and LBW infant outcomes may offer opportunities for intervention among this population.
Objective: We aimed to identify maternal risk factors for delivering LBW infants and describe infant 1) growth trajectories 2) mortality outcomes to 6 months of life in Pujehun and Western Rural Area Districts, Sierra Leone.
Design/Methods: This is a secondary analysis of the Mama Dutasi randomized trial comparing a package of nutritional and anti-inflammatory interventions with standard care for pregnant women with undernutrition defined by mid-upper arm circumference < 23 cm in Sierra Leone. Singleton live, presumed term by fundal height births with birth weight recorded were included. Weight, length, head circumference, and mortality were assessed at 72 hours, 6 weeks, 3 months, and 6 months. Growth parameters were converted to WHO z-scores. Multivariable logistic regression models were employed to calculate odds ratios for having a LBW infant adjusted for maternal study intervention and infant sex. Linear mixed models determined z-score growth trajectories for LBW versus non-LBW infants to 6 months of life and adjusted for maternal intervention. Cox proportional hazards regression for mortality were stratified by LBW status and adjusted for maternal intervention.
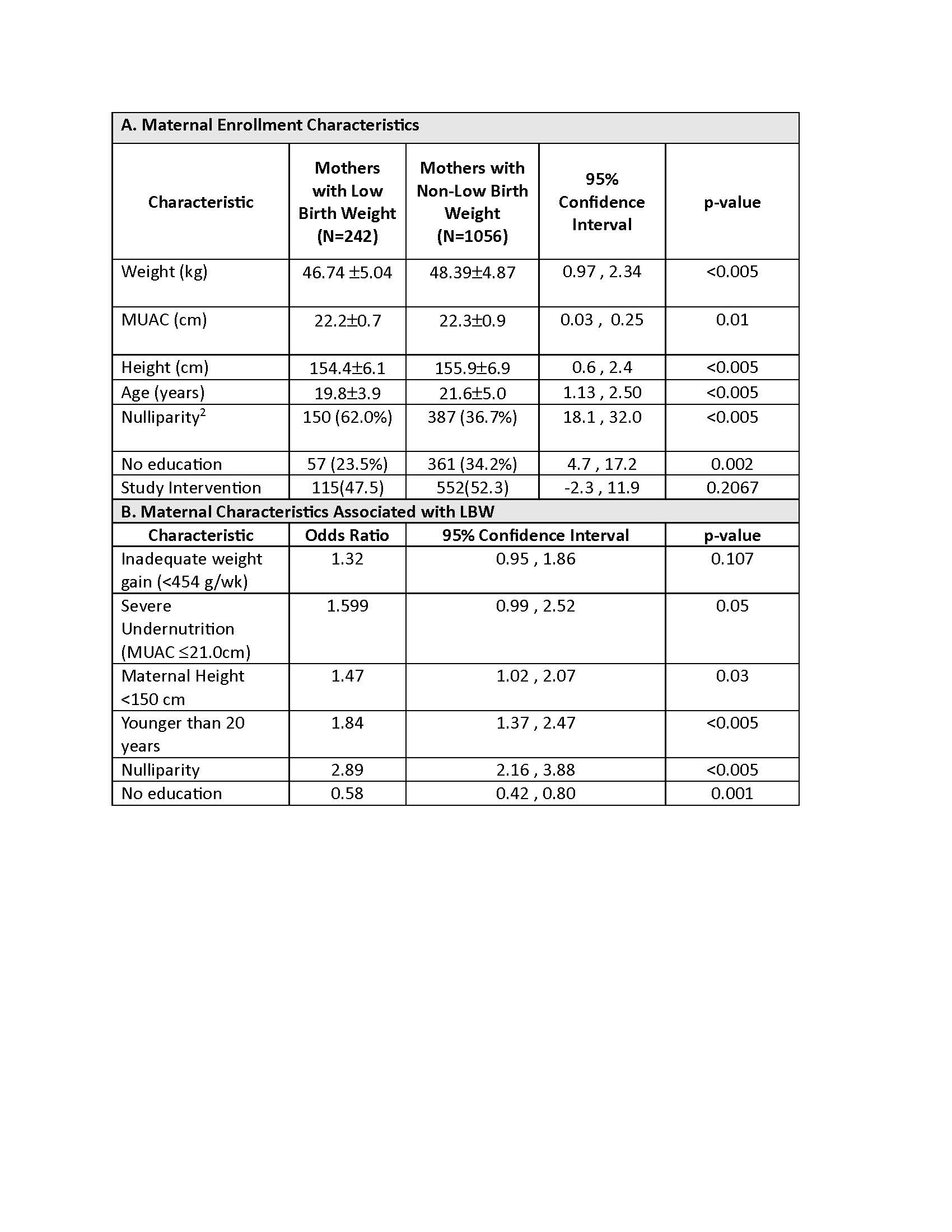
Results: Among 1298 infants, 242 (18.6%) were LBW. Being nulliparous (2.89; 95%CI 2.16, 3.88), < 20 years old (1.84; 1.37, 2.47), and < 150 cm tall (1.47; 1.02, 2.07) carried significantly elevated odds of having a LBW infant (Table 1).
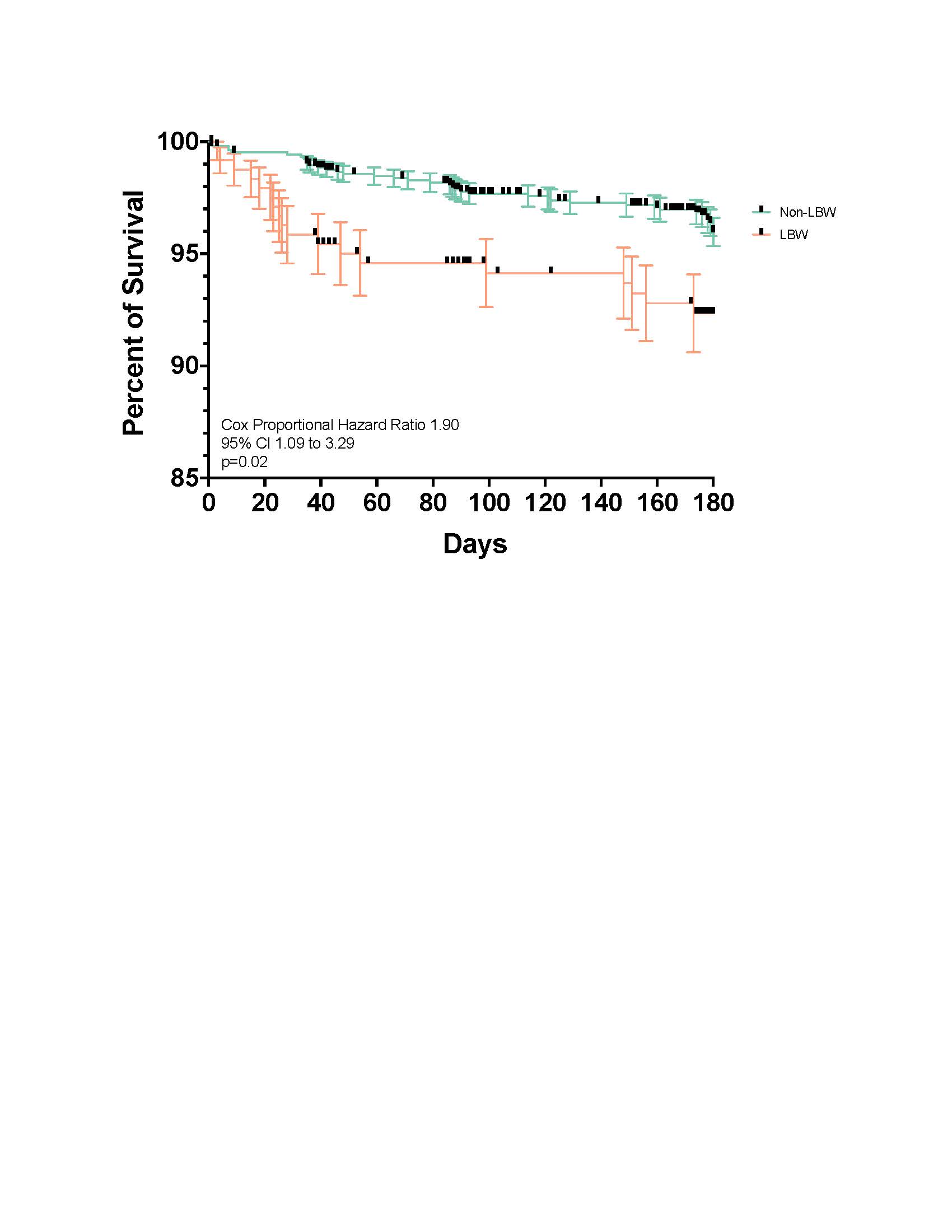
LBW infants had lower adjusted weight (-1.03; 95%CI -1.13, -0.92; p< 0.005), length (-0.72; -0.82, -0.63; p< 0.005), and head circumference (-0.73; -0.82, -0.64; p< 0.005) z-score change from birth to six months (Figure 1). LBW infants had an increased hazard of death at 6 months (1.90; 1.09, 3.29, p=0.02) when compared to non-LBW infants (Figure 2).
Conclusion(s): Women in Sierra Leone with undernutrition have a high rate of LBW infants. Maternal stunting, young age and nulliparity increase the risk of delivering a LBW infant. LBW infants’ growth z-scores decline substantially compared to non-LBW peers to 6 months and carry an increased hazard of mortality. Interventions are urgently needed to prevent LBW births among high-risk groups and support LBW infant growth.
.jpg)