Neonatology
Session: Neonatal Follow-up 3
530 - Association between Area Deprivation Index and Neurodevelopmental Outcomes and Follow-up in Extremely Preterm Infants.
Monday, May 6, 2024
9:30 AM - 11:30 AM ET
Poster Number: 530
Publication Number: 530.3172
Publication Number: 530.3172
.jpg)
Arpitha Y. Shenoy (she/her/hers)
Medical Student
University of Virginia School of Medicine
Fairfax, Virginia, United States
Presenting Author(s)
Background: The Area Deprivation Index (ADI) measures neighborhood disadvantage using American Census Survey data such as income, education, employment, and housing quality. In a multicenter cohort of extremely premature infants (EP, gestational age < 29 weeks), a higher national ADI percentile, or more deprivation, was associated with increased mortality and morbidity in the NICU (PMID: 37166800). These findings demonstrate how pervasively maternal deprivation affects infant outcomes.
Objective: To investigate associations between ADI and neurodevelopmental consultations, follow-up, and outcomes of EP NICU patients admitted to a level IV NICU with an inpatient Developmental Pediatrics consultation service and referral to an outpatient Early Development Clinic (EDC) and Early Intervention (EI) services.
Design/Methods: We collected clinical and ADI data for EP infants admitted in 2018-2020 and survived to hospital discharge. National ADI percentiles of infants were determined using the mother’s address recorded at delivery. We compared characteristics of infants above (high ADI) and below (low ADI) the national median ADI using Fisher's-exact tests and t-tests.
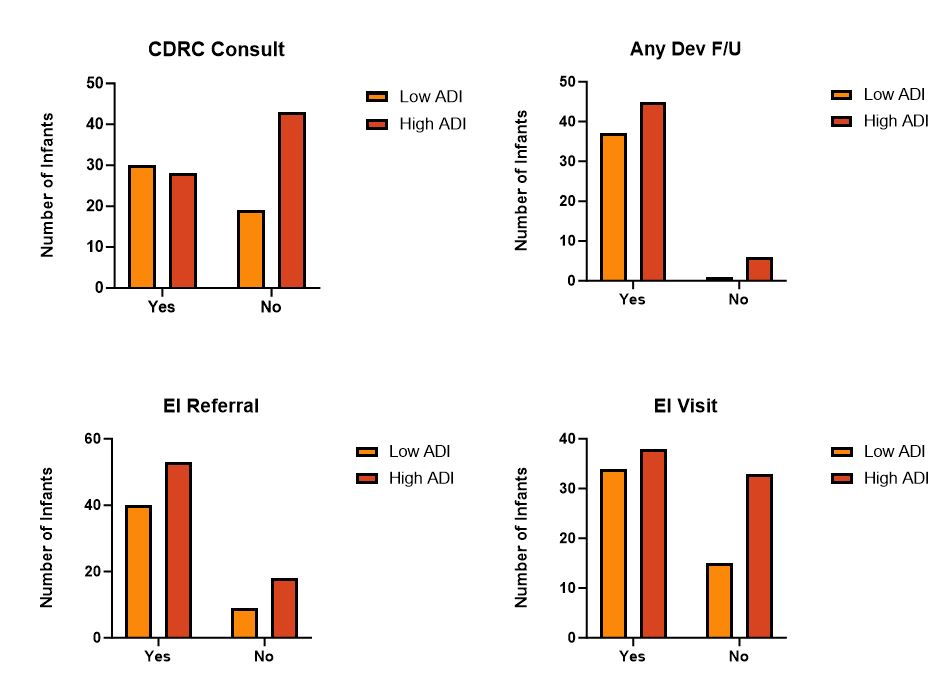
Results: We analyzed 132 infants, of which 120 had ADI data available. More infants had high ADI (71, 59%). Table 1 shows comparisons of high and low ADI infants and proportions with inpatient and outpatient developmental referral or follow-up. Infants with high ADI lived farther from the NICU and clinics, and were less likely to have an inpatient Developmental Pediatrics consult or outpatient EDC referral. Smaller proportions of high ADI infants had any EDC or EI visit, but these differences were not statistically significant. There was a higher proportion of Black infants from high ADI areas. Sex, ethnicity, and short-term outcomes were similar between ADI groups.
Conclusion(s): Area deprivation correlated with lower neurodevelopmental referral, Black race, and center distance from home, but not short-term outcomes. Trends toward lower follow-up rates for infants with low ADI warrant continued analysis.
.jpg)
.jpg)
