Health Equity/Social Determinants of Health
Session: Health Equity/Social Determinants of Health 7
299 - Mapping community assets and youth mental health: insights from a geospatial analysis
Sunday, May 5, 2024
3:30 PM - 6:00 PM ET
Poster Number: 299
Publication Number: 299.1843
Publication Number: 299.1843

Nicholas Szoko, MD (he/him/his)
Adolescent Medicine Fellow
UPMC Childrens Hospital of Pittsburgh
Pittsburgh, Pennsylvania, United States
Presenting Author(s)
Background: Socioenvironmental factors in youths’ neighborhoods and communities directly influence health. Existing measures of these determinants employ census-level indicators that often focus on areas of deficit, neglecting more granular community-level assets that may support adolescent well-being.
Objective: Our goal was to apply geographic information system (GIS) analyses to understand relationships between community-level assets and aspects of youths’ mental health.
Design/Methods: We used data from the Western Pennsylvania Regional Data Center (WPRDC), the 2020 Child Opportunity Index (COI) 2.0 database, and the 2018 Allegheny County Youth Risk Behavior Survey (YRBS). The WPRDC dataset included latitude/longitude data for >30,000 assets in Allegheny County, which were divided into eight categories. We calculated asset density in each zip code by summing the number of assets and dividing by the estimated population under 18. The COI includes three domains with indicators derived from census-level data: Education, Health & Environment, and Social & Economic. Mental health measures from YRBS included past 12-month feelings of hopelessness, non-suicidal self-injury (NSSI), and suicidal ideation (SI), operationalized as binary response variables (any/none). We used generalized linear mixed models to explore associations between asset density, COI, and each mental health measure while accounting for school-level clustering.
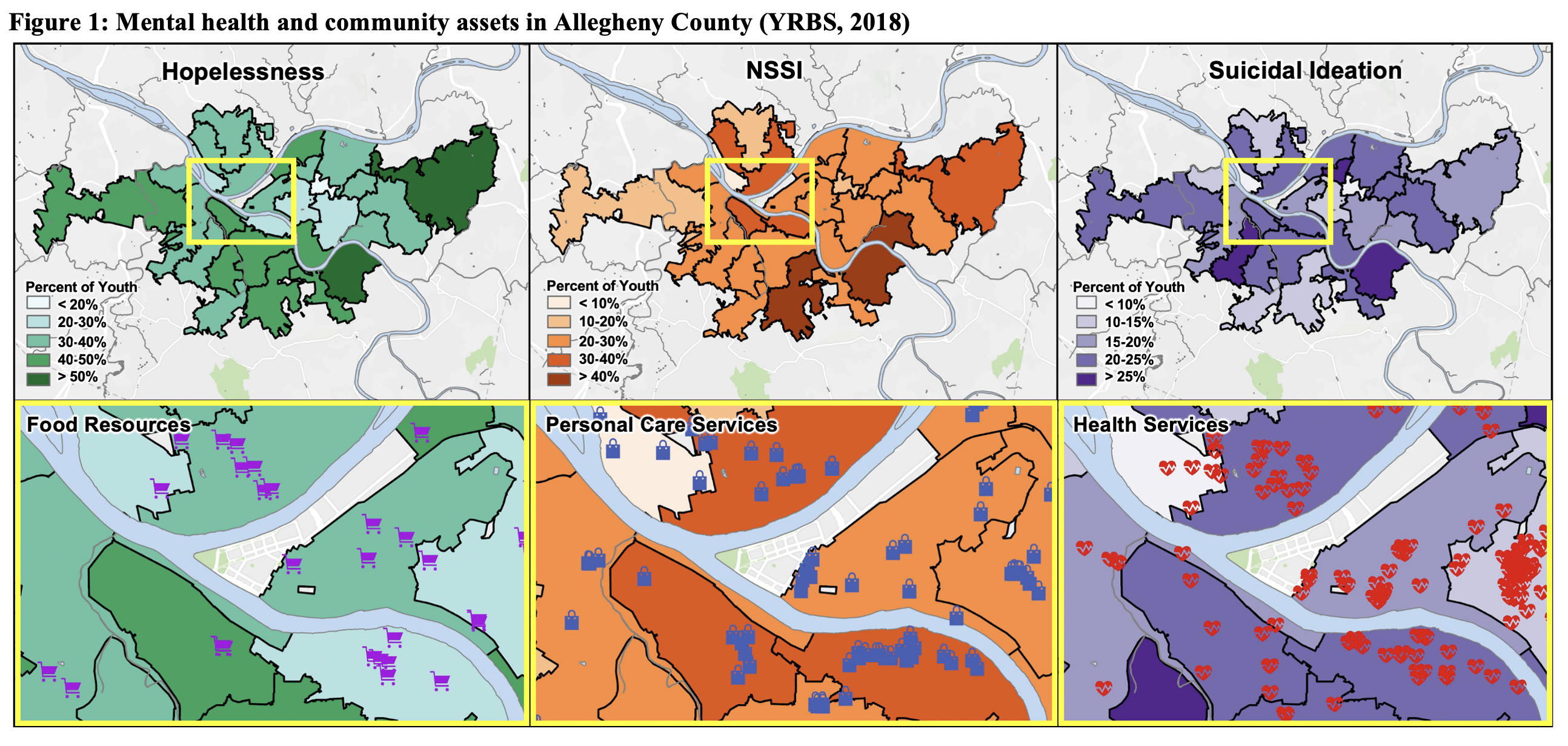
Results: 2,162 youth were included in the analysis (Table 1). Over a third (n=811, 37.5%) reported past 12-month feelings of hopelessness. NSSI and SI were also common (NSSI: n=587, 27.2%; SI: n=450, 20.8%) (Figure 1). Higher asset density was significantly associated with lower odds of hopelessness across four categories: Transportation (aOR=0.84 [0.71-0.98]), Health Services (aOR=0.72 [0.57-0.95]), Food Resources (aOR=0.79 [0.69-0.91]), and Personal Care Services (aOR=0.81 [0.69-0.95]) (Table 2). Higher COI was also significantly associated with lower odds of hopelessness (Health & Environment: aOR=0.90 [0.82-0.99]; Social & Economic: aOR=0.88 [0.81-0.96]; Overall: aOR=0.89 [0.81-0.97]). There were no significant relationships between asset density, COI, and other mental health measures.
Conclusion(s): We demonstrate significant associations between community assets and aspects of youths’ mental health. While there was some concordance with results obtained using census-derived metrics, our results offer a more granular understanding of community-level assets that centers community strengths in data analysis, interpretation, and dissemination.
.png)
.png)