General Pediatrics
Session: General Pediatrics 2
239 - Characterizing referrals to mental and behavioral health and community resources in an urban pediatric primary care practice
Friday, May 3, 2024
5:15 PM - 7:15 PM ET
Poster Number: 239
Publication Number: 239.203
Publication Number: 239.203

Nehaly S. Patel, MD (she/her/hers)
Resident Physician
UH Rainbow Babies & Children's Hospital
Presenting Author(s)
Background: Screening in pediatric primary care for social needs and behavioral health aims to increase access to needed services. However, it is unclear which characteristics or approaches are most likely to lead to successful uptake of referrals to such resources.
Objective: In an urban primary care pediatric practice, to describe patient characteristics and practice processes associated with acceptance of referrals to social and behavioral health resources.
Design/Methods: Retrospective review of SEEK (Safe Environment for Every Kid) screening and follow-up activities conducted during routine pediatric well-child visits for children 6 months to 6 years. Response activities as documented by the practice’s clinicians, early infant mental health specialist, social workers, and/or community health workers were linked to screen results. Records were excluded if SEEK screen was incomplete or if there was a duplicate caregiver screen from a sibling visit.
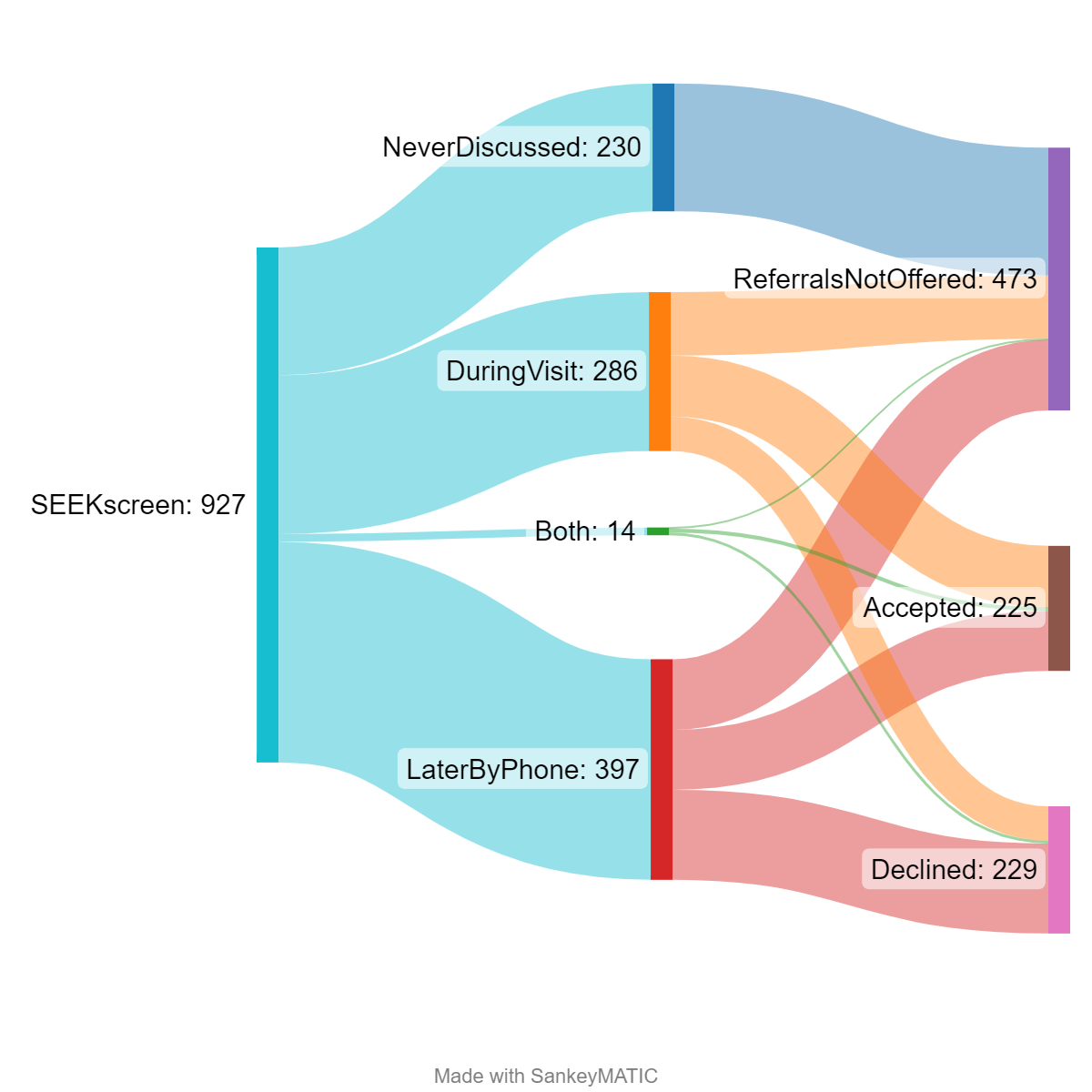
Results: Of 1,104 patients with SEEK screens completed Apr 2020–Sep 2022, 927 met inclusion criteria. Referrals were discussed at time of screening for 286 (“immediate”), and follow-up contact was attempted for 397 (“asynchronous,” median time from screen to follow-up 11 days); 14 had both forms of contact. Demographics and experience of social determinants of health were similar for those who accepted referrals and those who did not. Screen results were more often discussed if caregivers reported harsh punishment (p=0.036), stress (p < 0.001), or depression (p < 0.001). Discussion of SEEK screen included the offer of referral in 65% of cases; of caregivers who were offered referrals, 49% accepted at least one. For each additional topic endorsed, the odds of accepting referral increased by 25% (95%CI: 1.07, 1.47), accounting for covariates. Caregivers were significantly more likely to accept referrals if the conversation was immediate (p < 0.001). Mental or behavioral health services were the most common accepted referral (49%), followed by parenting groups (24%), community resources (20%), social work (7%), and medical-legal partnership (2%).
Conclusion(s): SEEK screening can be used to identify patients with unmet social and behavioral health care needs. Caregivers more often accepted referrals if more than one risk factor was identified, and if referral was offered immediately versus asynchronously. However, there was still significant uptake of referrals by phone after a routine pediatric well-visit, suggesting that multidisciplinary support in a primary care pediatric practice can provide needed support for families.
.jpg)
.jpg)
