Neonatology
Session: Neonatal Follow-up 4
556 - The Impact of Severe Brain Injury on the Trends of Gestational age-Related Neurodevelopmental Outcomes in Infants Born Very Preterm: A Population Cohort Study 2011-2020
Monday, May 6, 2024
9:30 AM - 11:30 AM ET
Poster Number: 556
Publication Number: 556.3166
Publication Number: 556.3166
- LW
Lan-Wan Wang, MD, PhD. (she/her/hers)
Attending physician
Chi Mei Medical Center
Tainan, Tainan, Taiwan (Republic of China)
Presenting Author(s)
Background: Infants born very preterm have high risks of severe neonatal brain injury (SNBI), which are highly associated with neurodevelopmental impairment (NDI) outcomes. However, the rates of NDI in very preterm survivors had no significant improvement over the past decades, despite declining rates of SNBI. Preterm infants without SNBI may still have risks of NDI potentially due to altered brain development affected by multiple adverse factors. It remains unknown whether preterm infants born at different gestational ages (GA) without SNBI have improving outcomes of NDI severity in the recent decade.
Objective: This study investigated whether the presence and absence of SNBI affected the trends of NDI outcome severity in infants born very preterm at different GA groups from 2011 to 2020.
Design/Methods: A population-based cohort study recruited 1091 infants born at GA < 31 weeks and admitted to neonatal intensive care units between 2011 and 2020 in Southern Taiwan. The NDI severity at 24 months of corrected age was classified into no/mild, moderate, and severe. The trends of neonatal morbidities, mortality, and NDI outcomes by birth epoch (2011-2015, 2016-2020) and GA group (22-25, 26-28, 29-30 weeks) were determined in infants with and without SNBI inclusion.
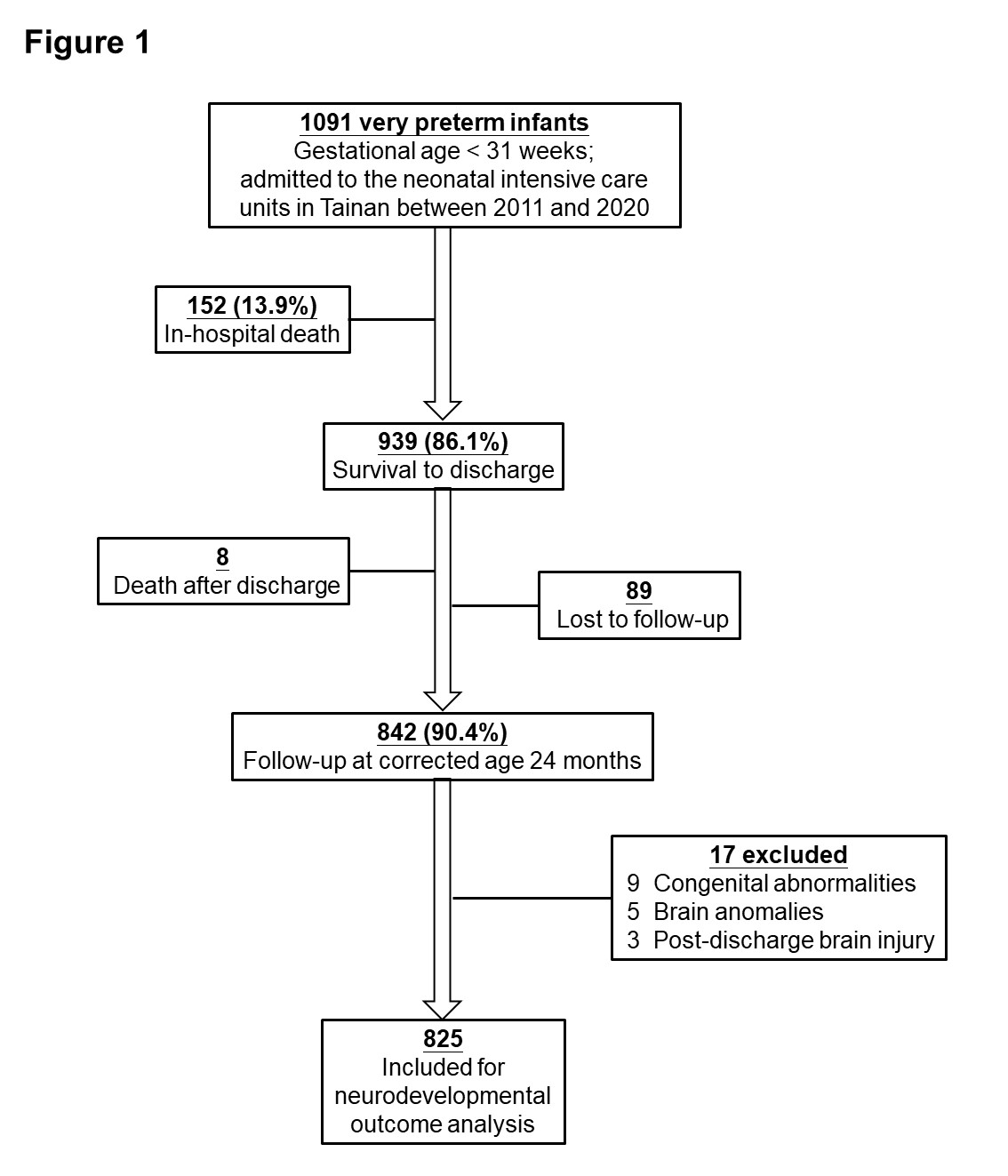
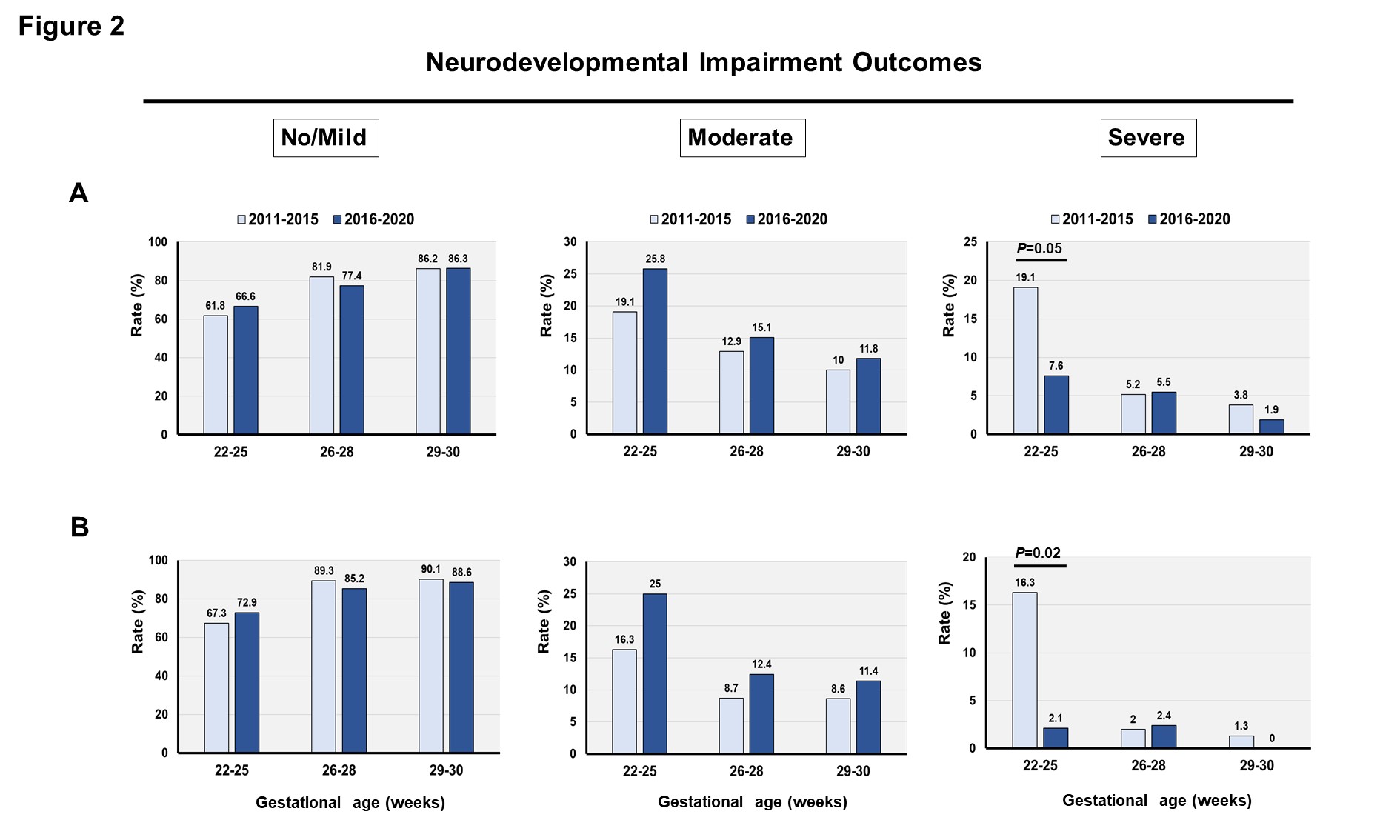
Results: There were increased antenatal steroids use, lower rates of extrauterine growth restriction, and higher maternal education levels and familial socioeconomic status over time. The rates of neonatal morbidities and mortality had no temporal changes. Among the 825 infants who were included for neurodevelopmental outcome analysis (Figure 1), there were no temporal changes in the distribution of no/mild, moderate and severe NDI outcomes in the GA 26-28 and 29-30 groups with (Figure 2A) and without (Figure 2B) inclusion of infants who had SNBI; whereas infants in the GA 22-25 group had decreased rates of severe NDI from 19% to 8% across epochs (Figure 2A), particularly in those without SNBI (from 16% to 2%, Figure 2B). Relative to the occurrence in Epoch 2011-2015, the risk of severe NDI was significantly reduced in Epoch 2016-2020 (adjusted relative risk 0.39, 95% confidence interval 0.16-0.96) for infants born at GA 22-25 weeks, and the risk dropped even lower in these infants without SNBI (0.12, 0.02-0.84).
Conclusion(s): For infants born at GA 22-25 weeks near the limit of viability, there was a decreasing trend of severe NDI at corrected age 24 months in the recent decade, particularly in infants without SNBI. The improvement might be attributed to better care in the perinatal/neonatal periods and after discharge.