Nephrology
Session: Nephrology 4
24 - Kidney disease factors among American Indian Youth: Strong Heart Family Study
Sunday, May 5, 2024
3:30 PM - 6:00 PM ET
Poster Number: 24
Publication Number: 24.1868
Publication Number: 24.1868
Reya Mokiao, MD, MS
Acting Assistant Professor
Seattle Children's Research Institute and University of Washington School of Medicine
Seattle, Washington, United States
Presenting Author(s)
Background: Kidney disease disproportionately affects American Indians (AI), yet there is limited data on risk and/or protective factors for kidney health in AI youth.
Objective: To examine the association of health behaviors and factors (physical activity, diet quality, smoking, body mass index, dyslipidemia, diabetes mellitus, hypertension, cardiovascular disease (CVD), social support, and achievement of a modified American Heart Association Life’s Essential 8) with kidney injury (prevalent and incident albuminuria) and dysfunction (low estimated glomerular filtration rate (eGFR) among AI youth.
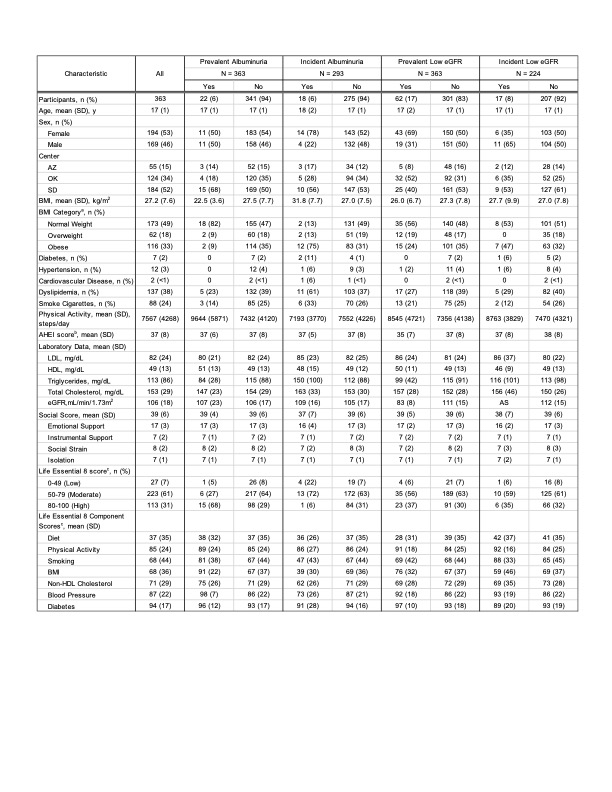
Design/Methods: The study population included youth participants (age 14-20y, n= 363, mean age 17 ± 1y, 53% female) from the Strong Heart Family Study, a longitudinal study of CVD and its risk factors among AIs from 12 tribes. Participants completed two exams (baseline: 2001-2003; follow-up 2007-2009) with up to 8 years of follow-up. Primary exposures are noted above. Assessments and instruments included: physical activity (by pedometer), diet quality (by the Alternative Healthy Eating Index 2010), social support score (by the American Indian Service Utilization and Psychiatric Epidemiology Risk and Protective Factors Project questionnaire), and healthy lifestyle (by a modified Life’s Essential 8 score which included all components except sleep). Primary outcomes were prevalent and incident albuminuria (urine albumin to creatinine ratio of 30mg/g or greater); prevalent and incident low eGFR ( < 90 ml/min/1.73m2 using CKiD U25 equation). Relative risks could not be calculated due to small sample size. Results presented are descriptive and unadjusted. Total sample size for each outcome vary due to missingness.
Results: Approximately 6% of AI youth had prevalent (n=22) or incident (n=18) albuminuria; 17% had prevalent (n=62) and 8% incident (n=17) low eGFR (Table 1). Among AI youth in the Strong Heart Family Study, albuminuria, incident low eGFR and kidney disease risk factors were uncommon except for obesity, dyslipidemia and smoking cigarettes. Overall diet quality was poor, but social support was high. Majority of AI youth (61%) had moderate cardiovascular health based on modified Life’s Essential 8 scores. Those with incident albuminuria (vs those without albuminuria) had worse risk factors (higher BMI, more dyslipidemia) and lower cardiovascular health based on modified Life’s Essential 8 scores at baseline.
Conclusion(s): Research is needed in large samples of AI youth to examine health behaviors and factors associated with albuminuria to identify areas for intervention in this high-risk population.