Clinical Bioethics
Session: Clinical Bioethics
427 - How would the general population have allocated pediatric intensive care resources to adults in the context of the COVID-19 pandemic?
Sunday, May 5, 2024
3:30 PM - 6:00 PM ET
Poster Number: 427
Publication Number: 427.1874
Publication Number: 427.1874
Naomi Singh, RN, BSN (she/her/hers)
Adult emergency nurse, pediatric emergency nurse, flight nurse
Hôpital de Sacré-Coeur de Montréal, CHU Sainte-Justine
saint-hubert, Quebec, Canada
Presenting Author(s)
Background: An ethical consensus regarding how to allocate pediatric intensive care (PICU) resources in the context of the COVID-19 pandemic, which disproportionately affected adults, has not been reached. Understanding local social values is essential to inform the design and implementation of prioritization protocols.
Objective: To explore the general population’s perceptions on the allocation of PICU resources between children and using said ressources to treat adults during the COVID-19 pandemic in Canada.
Design/Methods: An online democratic deliberation (DD) exercise was held with adults from Ontario and Quebec, Canada. Participants took part in two days of information sessions and deliberations; consensus was not sought. Questionnaires investigating participants’ values and preferences on the allocation of PICU resources to adults were completed before and after the DD. Questionnaires were developed by an interdisciplinary team of researchers, and included multiple choice, Likert scale items, and open-ended items. Questionnaire analyses included descriptive reports of frequencies; participants’ pre- and post-DD responses to Likert scales were compared using Wilcoxon sign tests, using SPSS (v.24, IBM Inc).
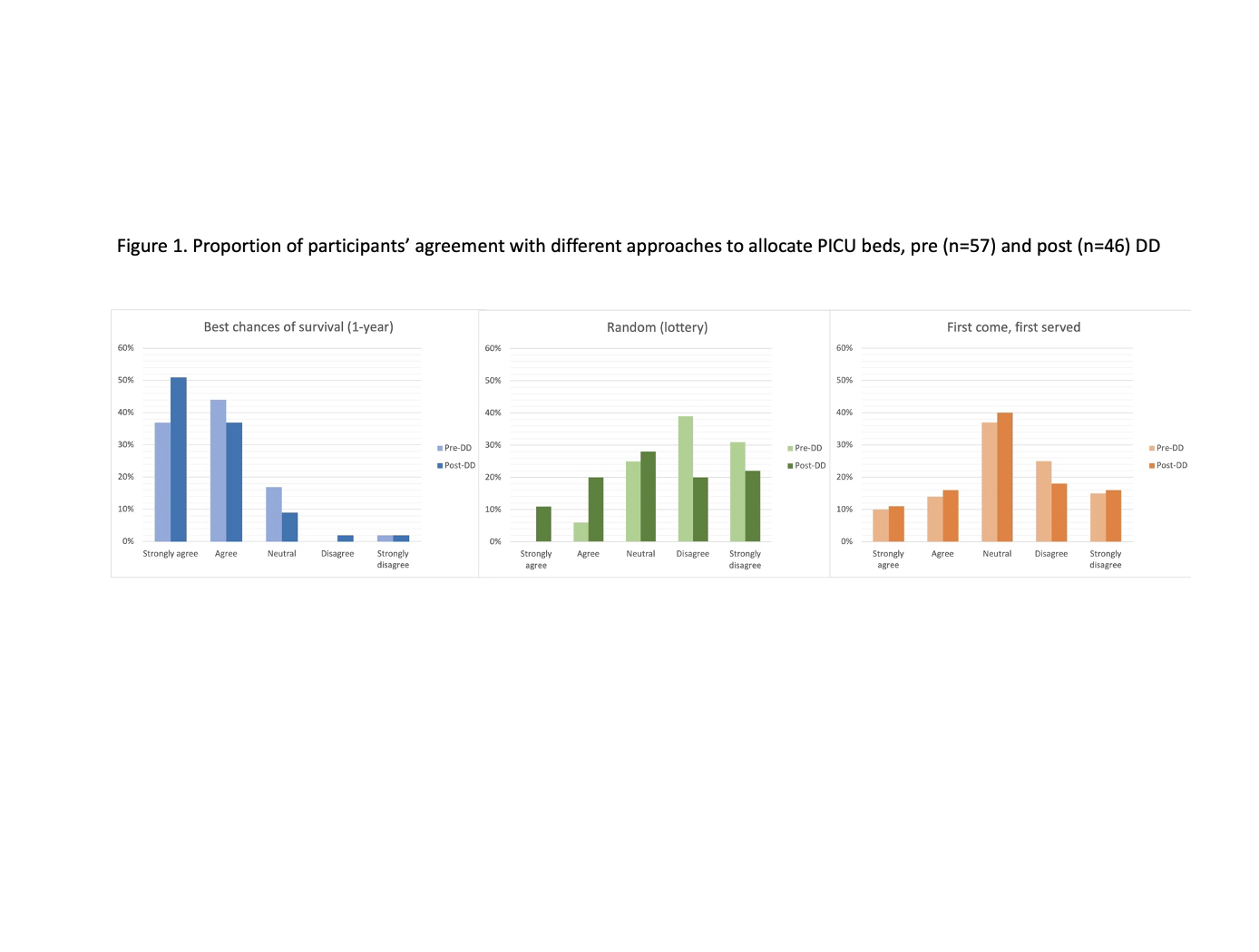
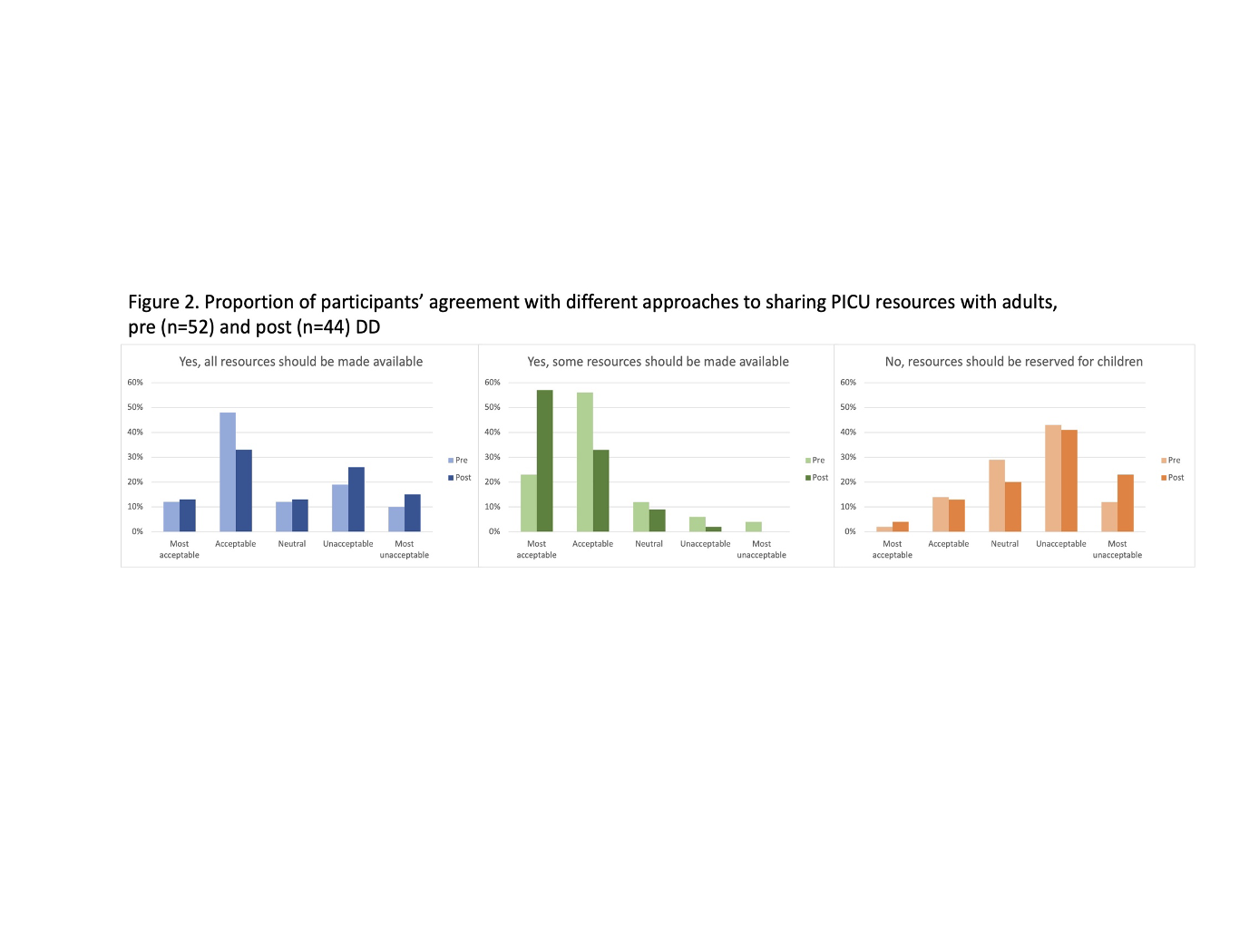
Results: In the spring of 2022, 57 participants participated in day 1 and completed the pre-DD questionnaire, while 47 participated in both days and completed the pre- and post-DD questionnaires. Participants’ demographic information and rationale for participating in the DD are presented in Table 1. Following the DD, there was a significant increase in the acceptability of using a pediatric triage protocol to allocate PICU resources amongst children (84% pre-DD to 93% post-DD, p=0.049). Participants were asked to rate the acceptability of three allocation principles to allocate a PICU resource between children (Figure 1). There was a significant increase in the proportion of participants who “agreed/strongly agreed” with the use of random allocation after the DD (6% ped-DD to 33% post-DD; p=0.006). Participants were also asked the acceptability of strategies to allocate PICU resources to adults (Figure 2). Most believed that it was “acceptable/most acceptable” to share some pediatric resources before and after the DD and this proportion increased significantly following the DD (79% pre-DD and 90% post-DD; p=0.001) (Figure 2).
Conclusion(s): This study provides insight into how the general population in Canada assesses the ethical tension between maximising the use of PICU resources while also protecting said resources. It also demonstrated the impact of a DD on participants’ understandings of this issue.
.png)
