Children with Chronic Conditions
Session: Children with Chronic Conditions 3
292 - Fostering Holistic Care for Children with Medical Complexity through an Interprofessional Family-Led Narrative Medicine Workshop Series
Friday, May 3, 2024
5:15 PM - 7:15 PM ET
Poster Number: 292
Publication Number: 292.243
Publication Number: 292.243

Cara L. Coleman, JD, MPH (she/her/hers)
Instructor of Medical Education
University of Virginia School of Medicine
Lorton, Virginia, United States
Presenting Author(s)
Background: Narrative medicine is an educational strategy involving close reading and reflective writing, which has been shown to improve communication and develop professional identity. Children with medical complexity (CMC) rely on comprehensive care of an interprofessional team, inclusive of families. Leveraging narrative medicine with clinicians and families who care for CMC may facilitate shared understanding and foster a holistic approach to care.
Objective: To explore the impact of participation in an interprofessional, family-led narrative medicine workshop series on participants' perspectives on the nature of complex care and role of the care team.
Design/Methods: Clinicians and family leaders who care for CMC were recruited via a complex care email listserv to participate in a 6-week online narrative medicine workshop series. Complex care entrustable professional activities served as a conceptual framework, with each workshop involving close reading of a text aligned with an essential clinical activity in the care of CMC (i.e. feeding tube care, evaluating pain/irritability), reflective writing, and facilitated discussion with a family leader. Participants were asked to define the clinical activity before and after each workshop. Electronic surveys after each workshop asked about whether learning objectives were met and key takeaways. Transcripts of the workshops were analyzed via inductive thematic analysis.
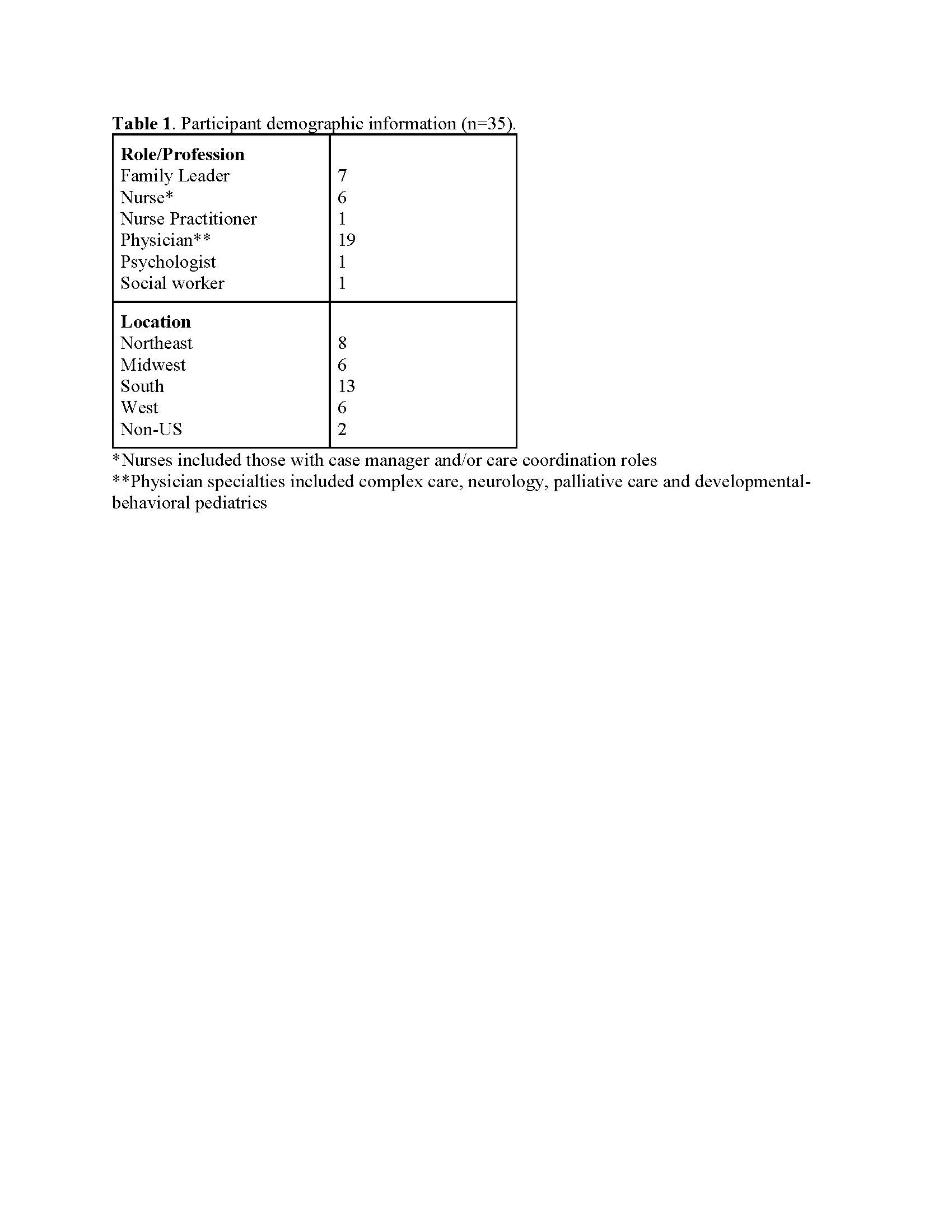
Results: Since July 2023, 3 cohorts of 11-12 participants each were enrolled (Table 1). To date, 15 of 18 workshops have been completed, with a median of 9 participants per workshop. All participants agreed or strongly agreed that learning objectives were achieved. Definitions of clinical activities and reflections included new concepts and understandings. Preliminary themes included “normalcy” (i.e. addressing ableism), role on the care team (i.e. recognizing limitations), complexity of decision-making (i.e. navigating uncertainty), emotions (i.e. grief and frustration), psychosocial experiences (i.e. sense of connection), and perspective-taking (i.e. clinicians considering patient/family viewpoints) (Table 2). Data analysis is ongoing.
Conclusion(s): A novel family-led educational intervention was feasible for a broad range of clinicians and family leaders and yielded rich discussion of shared experiences in providing team-based care for CMC. Narrative medicine can be a valuable educational strategy for complex care teams to facilitate mutual understanding of roles and foster a holistic approach to clinical care of CMC.
.jpg)
