Neonatology
Session: Neonatal Quality Improvement 2
397 - Implementation of standardized social determinants of health screening and referral among 5 safety-net NICUs in Massachusetts
Sunday, May 5, 2024
3:30 PM - 6:00 PM ET
Poster Number: 397
Publication Number: 397.1895
Publication Number: 397.1895

Margaret Parker, MD, MPH
Professor of Pediatrics
UMass Memorial Children's Medical Center
Worcester, Massachusetts, United States
Presenting Author(s)
Background: Social determinants of health screening (SDOH) is routine in many pediatric office settings. This practice has not yet come to scale in the neonatal intensive care unit (NICU) setting, despite high prevalence of low-income families with adverse SDOH.
Objective: We aimed to increase SDOH screening and referral using standardized tools among families of NICU infants admitted 7 days by 30% of baseline from 01/01/2023 to 10/1/2023 at 5 safety-net hospitals.
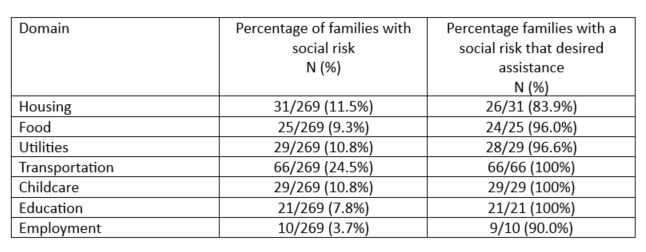
Design/Methods: We conducted a multi-site quality improvement (QI) collaborative in Massachusetts. From 10/2022 to ~2/2023, we created multi-disciplinary teams, chose center-specific SDOH screening tools and adapted them to the NICU context. Concurrently, we created community resources guides that contained information regarding available resources. Beginning in ~3/2023, we used plan do study act cycles to integrate routine SDOH screening into existing NICU workflow and report results in discharge summaries, in order to convey information to out-patient providers. We assessed families’ social risks for housing, food, utilities, transportation, childcare, education and employment and whether families desired assistance with any social risk identified. Our main outcome was percent of eligible families approached for screening. Our secondary outcomes were percent of infants with screening results in discharge summaries and identified social risks among families screened, and percent of families with an indicated desire for assistance among those with a social risk. Our balancing measure was percent of families that declined screening. We examined our main outcome stratified by maternal race/ethnicity and primary language to determine whether there were inequities in improvements.
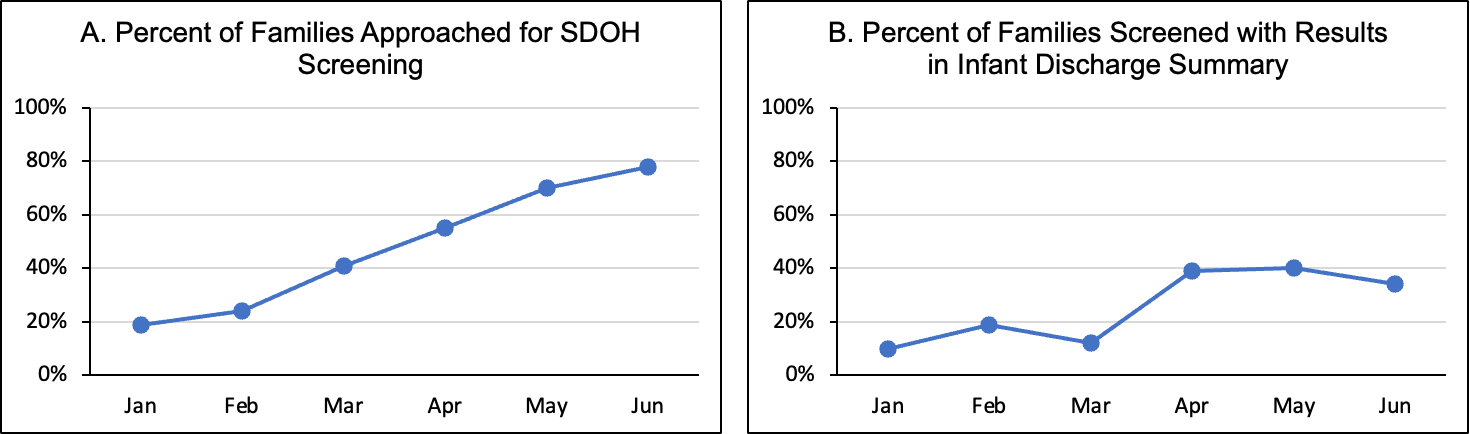
Results: We present data on 569 infants admitted 7 days from 1/01/23-6/30/23. 273 of 569 (47%) families were approached for SDOH screening. Among 273 families approached, 4 (1.4%) declined and 269 (98.6%) were screened. The rate of families that were approached increased from 19% to 78% in 6 months (Figure). Among families screened, the rate of screening results in the discharge summary increased from 10% to 34% (Figure). Rates of indicated social risks and desire for assistance are shown in the Table. We did not find differences in our main outcome according to social factors.
Conclusion(s): Implementation of SDOH screening and referral using standardized tools within the workflow of safety-net NICUs is feasible. Social risks were highly prevalent and nearly all families desired assistance.