Health Equity/Social Determinants of Health
Session: Health Equity/Social Determinants of Health 2
455 - Surveillance of Healthcare Equality and Implicit Bias through Incident Reports
Friday, May 3, 2024
5:15 PM - 7:15 PM ET
Poster Number: 455
Publication Number: 455.250
Publication Number: 455.250

Francesca Tuquynh Le, MD
Neonatology Fellow, PGY-6
Harbor UCLA/ Cedars-Sinai Medical Center
Los Angeles, California, United States
Presenting Author(s)
Background: Implicit bias has been identified as a significant factor contributing to disparities in healthcare quality and outcomes. Despite its importance, the full scope of racial and ethnic disparities within healthcare systems is not well-defined. While hospitals use incident reporting systems to monitor adverse events, these systems are inherently prone to biases.
Objective: The aim of this study was to investigate our incident reporting database to assess healthcare disparities within a Level IV Neonatal Intensive Care Unit (NICU).
Design/Methods: We conducted a retrospective review at a single site, examining all NICU incident reports submitted to the Cedars-Sinai Safety Event Reporting System (CS-SAFE) between January 2020 and June 2023. The study included infants with comprehensive data on mother-baby dyads who were admitted to the NICU. We compared the characteristics of infants with reported adverse events to those without. We collected demographic variables, including maternal age, gestational age (GA), birth weight (BW), and maternal body mass index (BMI) at delivery. Additionally, we recorded the infant's race/ethnicity, length of newborn stay, and insurance status (public vs. private). To account for confounding factors, we conducted multivariable logistic regression analysis.
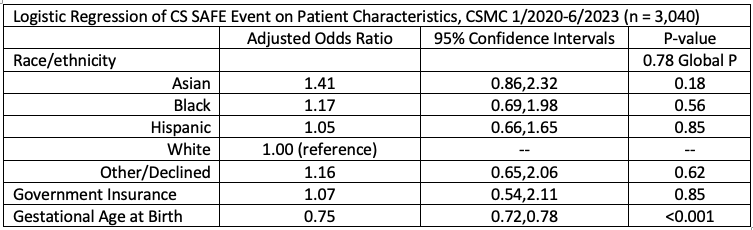
Results: Our analysis encompassed 3,340 infants, including 173 with adverse events. Black, Asian, and Hispanic infants were overrepresented in the group with adverse events compared to White infants (Table 1, p= 0.03). However, this difference was mitigated and no longer statistically significant (Table 2, p= 0.78) in the multivariable logistic regression model, which accounted for gestational age at birth. No significant differences were observed between the two groups concerning maternal age, BMI, and insurance status.
Conclusion(s): Our examination of the incident reporting database, which encompasses both voluntary and mandatory reports, found no substantial disparities in NICU adverse event rates during the study period. These mixed reporting systems, given their comprehensive nature and accessibility, show promise as tools for identifying and addressing healthcare disparities. Nevertheless, challenges such as selective reporting biases might skew the true representation of disparities. Future research should evaluate the accuracy and reliability of these systems in genuinely capturing and reflecting equitable incident occurrences.
.png)