Health Equity/Social Determinants of Health
Session: Health Equity/Social Determinants of Health 4
252 - Disparities In Pediatric Emergency Department Revisits Within 7 Days By Disease Process
Saturday, May 4, 2024
3:30 PM - 6:00 PM ET
Poster Number: 252
Publication Number: 252.1463
Publication Number: 252.1463

Sagar D. Mehta, MD (he/him/his)
Pediatric Emergency Medicine Fellow
Emory University School of Medicine
Atlanta, Georgia, United States
Presenting Author(s)
Background: Minoritized pediatric populations and children from lower socioeconomic groups experience higher rates of emergency department (ED) revisits than White children and those with higher socioeconomic status. There is not a comprehensive understanding of disparities in ED revisit rates by disease processes, which could provide a framework for targeted interventions toward health equity.
Objective: To identify disease processes for which patients experience the greatest rates of ED revisit disparities by race, ethnicity, preferred language, insurance, and Childhood Opportunity Index (COI).
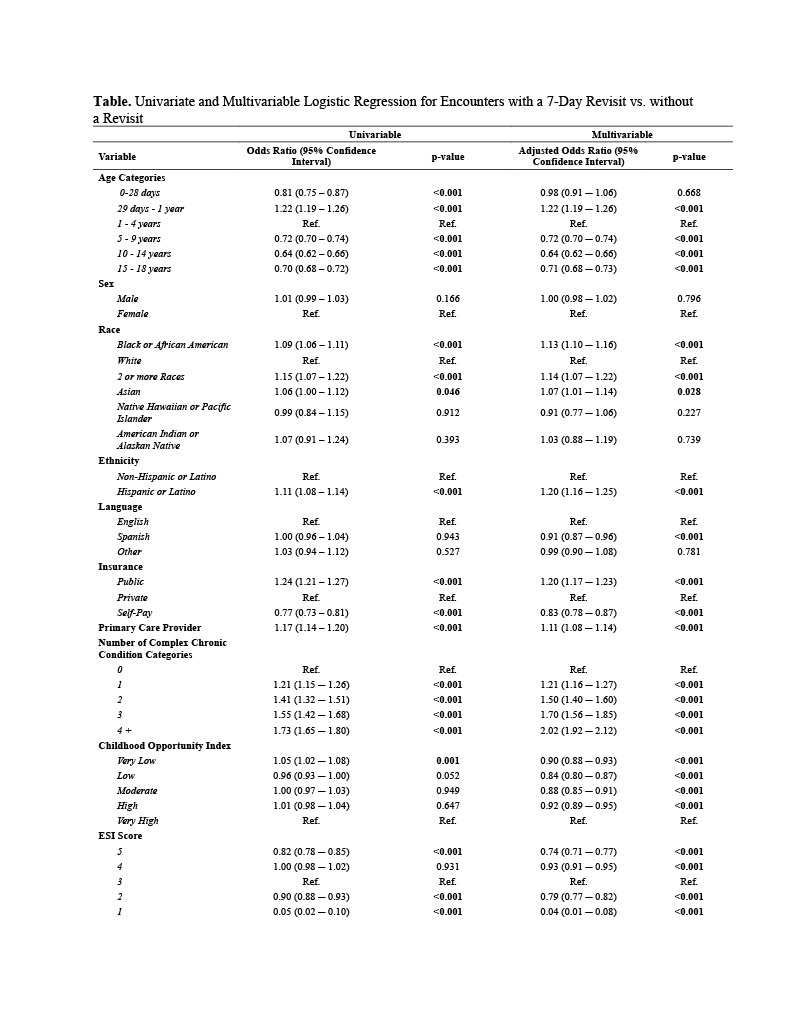
Design/Methods: We performed a retrospective, cross-sectional study of ED visits at a large comprehensive health system encompassing three EDs and capturing all representative demographic groups in the Atlanta metro region. We included all pediatric (i.e., aged 0-18 years) ED encounters that led to a discharge home (2018-2022). We excluded encounters among patients aged >18 years and those resulting in hospital admission or transfer at the first ED visit. The primary outcome was ED revisit within 7 days of a prior ED visit. We assessed the relationship between patient demographics (race, ethnicity, preferred language, insurance, COI), diagnoses, and the outcome of ED revisit within 7 days using bivariate and multivariable logistic regression. Diagnoses were categorized according to the PECARN Diagnosis Grouping System.
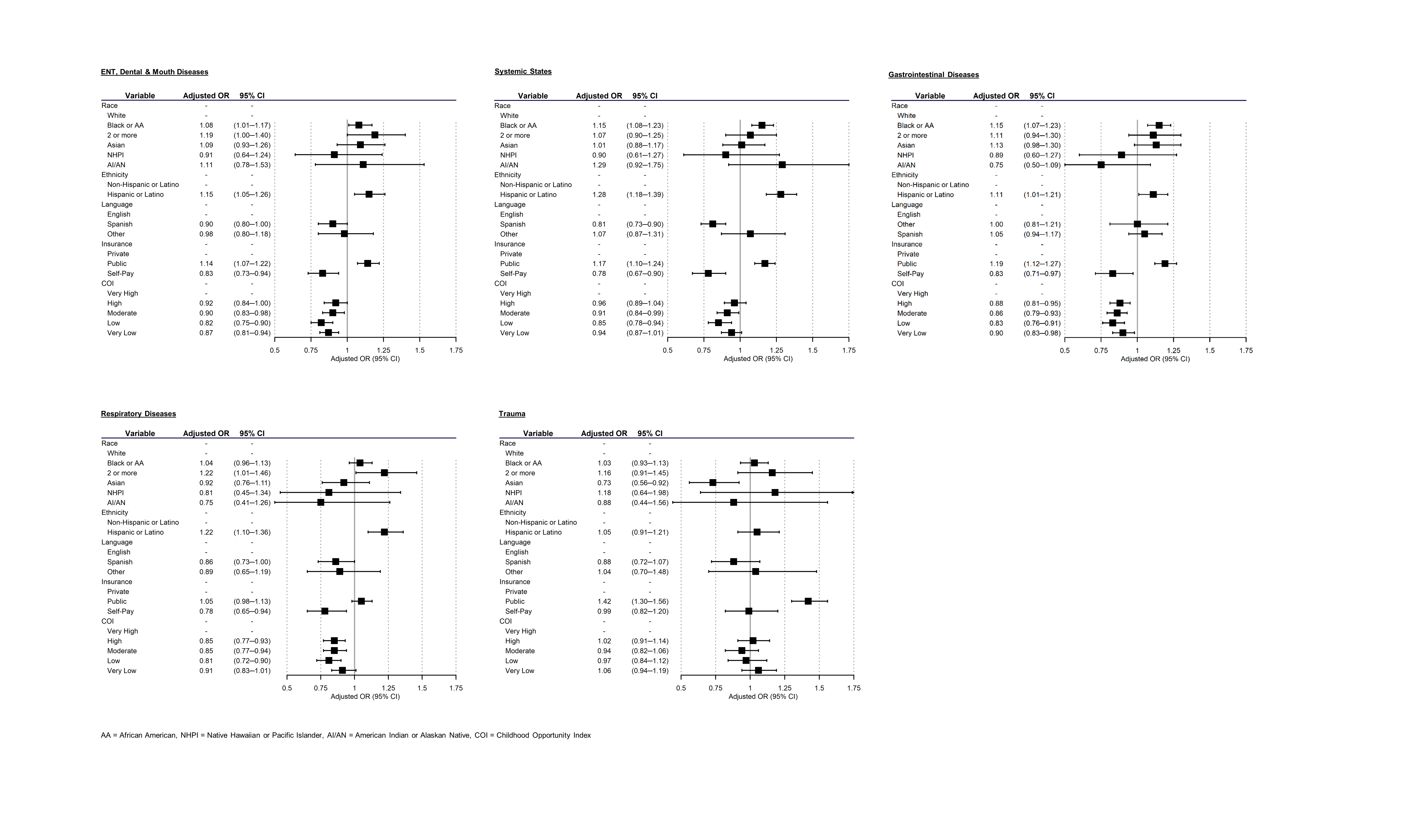
Results: There were 1,008,651 total ED encounters included and 52,176 (5.2%) had an ED revisit within 7 days. In the multivariable analyses, patients who identified as Black, Asian, Multiracial, Hispanic, those who had public insurance, and those with least one complex chronic condition had greater odds of ED revisit (Table). Spanish-speaking patients, those with self-paying insurance, and those living in lower COI level neighborhoods had lower odds of revisits. Black patients had higher adjusted odds of revisits for ENT/Dental/Mouth Diseases, Gastrointestinal Diseases, and Systemic States but not for Respiratory Diseases or Trauma (Figure). Hispanic patients had greater adjusted odds of revisits for the most common disease categories except for Trauma. Patients on public insurance had greater adjusted odds of revisits for the most common disease categories except for Respiratory Diseases.
Conclusion(s): Health disparities in ED revisits exist for certain populations and vary by disease process. It is crucial to develop disease-focused interventions to reduce the burden of ED revisits for minoritized and other populations at risk.