Health Equity/Social Determinants of Health
Session: Health Equity/Social Determinants of Health 3
465 - Inclusion of Communities Speaking Languages Other Than English (LOE) in Research: Exploring Barriers, Facilitators, and Recommendations
Friday, May 3, 2024
5:15 PM - 7:15 PM ET
Poster Number: 465
Publication Number: 465.254
Publication Number: 465.254
Henry Hoffman, BA (he/him/his)
Medical Student
University of Pittsburgh School of Medicine
Pittsburgh, Pennsylvania, United States
Presenting Author(s)
Background: Communities who speak languages other than English (LOE) are growing and constitute 9% of the U.S. population, but LOE inclusion in pediatric health research remains inadequate. While LOE exclusion hinders research generalizability and furthers inequity, little work has explored researcher views on LOE inclusion, barriers, and strategies to promote language justice. This is critical in new-growth immigrant communities like our region with growing LOE populations but insufficient bilingual services.
Objective: This study aims to assess researcher views around practices, barriers, and facilitators of LOE inclusion, and generate strategies to make research more inclusive.
Design/Methods: We conducted a cross-sectional study of PIs and coordinators from our institution who conducted human subjects research in the past 5 years. Survey questions, drafted with input from community partners, assessed past work with LOE participants, inclusion barriers and facilitators, demographics, and open-ended recommendations. Recruitment occurred via department emails, research listservs, an online recruitment repository and word of mouth. Data collection was via an anonymous Qualtrics survey that took 15 minutes to complete. Data cleaning removed incomplete surveys and bots. Descriptive data analysis assessed frequencies and means; qualitative data was coded and analyzed thematically. This study was IRB approved.
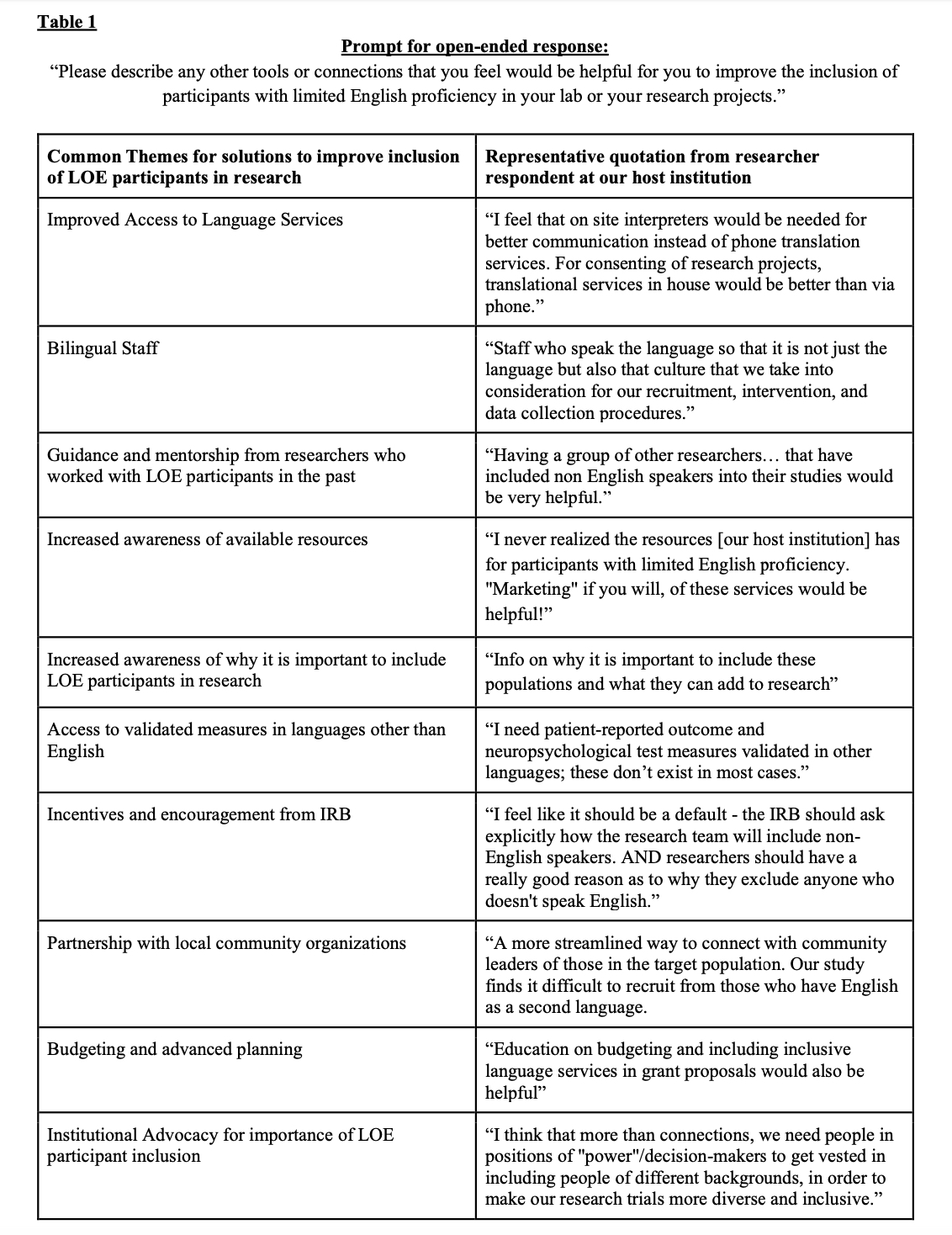
Results: 339 participants completed the survey (38% PIs, 63% coordinators). Most identified as white (74%) and cisgender females (78%) and conducted research in clinical (71%), health services (20%), or population health (18%) settings. 50% worked with LOE participants in the last 5 years; of those who had, 38% did not include LOE in their inclusion criteria, adjusting protocols after studies began, and 64% worked with LOE in < 50% of their studies. Researchers listed lack of bilingual staff, poor knowledge of best practices, language resource access, scheduling, and budgeting as barriers to inclusion. Researchers noted IRB training (76%), help finding language services (75%), validated LOE measures (74%), and access to interpreters (82%) would help improve inclusion. Table 1 includes qualitative themes and relevant quotations.
Conclusion(s): This study clarifies practices and barriers that hinder LOE inclusion in research, yet most barriers stem from knowledge gaps or poor advanced planning, which are easy to remedy. Improving knowledge of best practices, resource access, and preparing to work with LOE populations is vital to boost research inclusion in our region and similar immigrant communities nationwide.