Medical Education
Session: Medical Education 2
526 - Assessing the Efficacy of a Novel Online Module Outlining Escalation of Respiratory Support for Medical Students on Pediatrics Clerkship Rotations
Friday, May 3, 2024
5:15 PM - 7:15 PM ET
Poster Number: 526
Publication Number: 526.269
Publication Number: 526.269

Vidya Menon, MD (she/her/hers)
Chief Resident
Emory University School of Medicine
Atlanta, Georgia, United States
Presenting Author(s)
Background: Respiratory distress requiring escalation in respiratory support is a commonly encountered clinical scenario in pediatrics. There are many in-depth educational resources focused on this topic, but limited data on self-directed resources for clerkship-level medical students.
Objective: This study aims to assess the efficacy of an educational module outlining escalation in pediatric respiratory support for clerkship-level medical students.
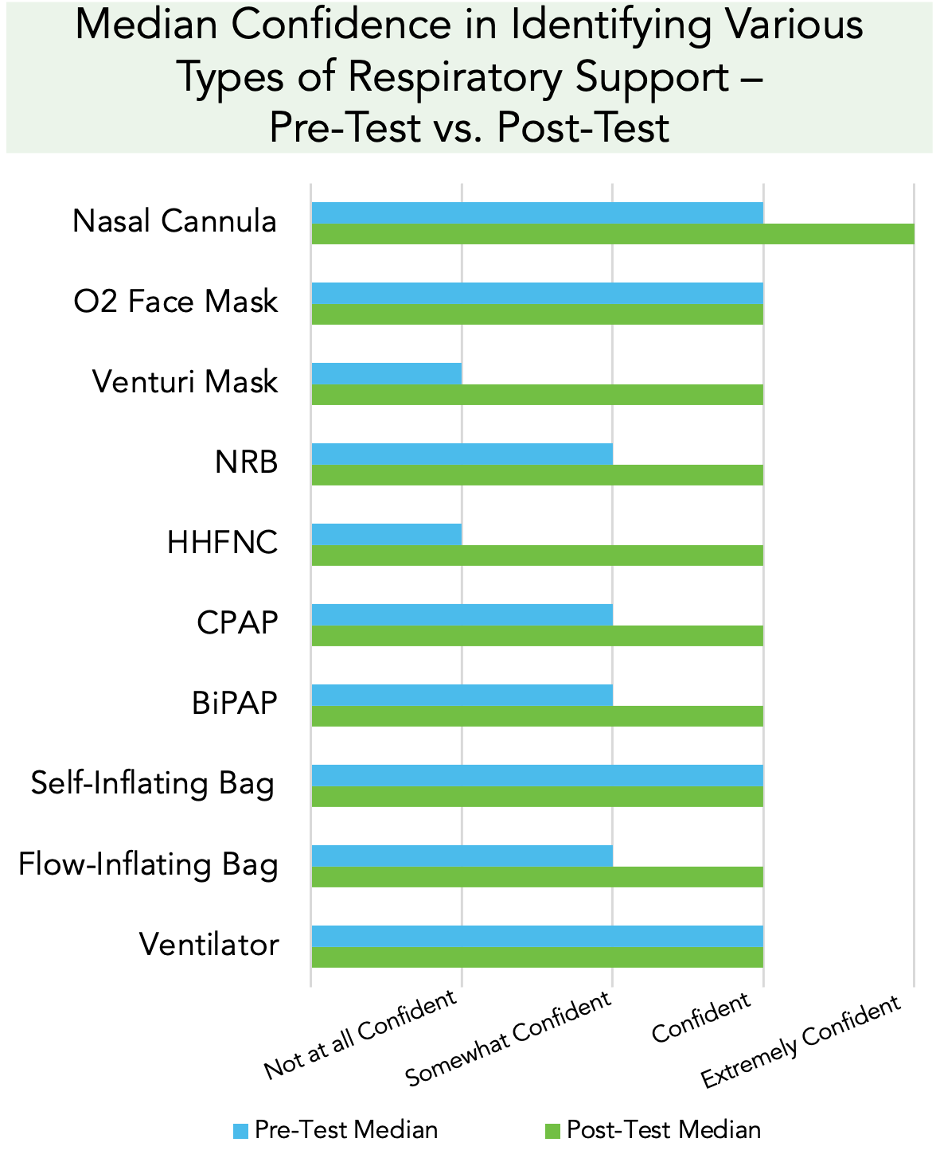
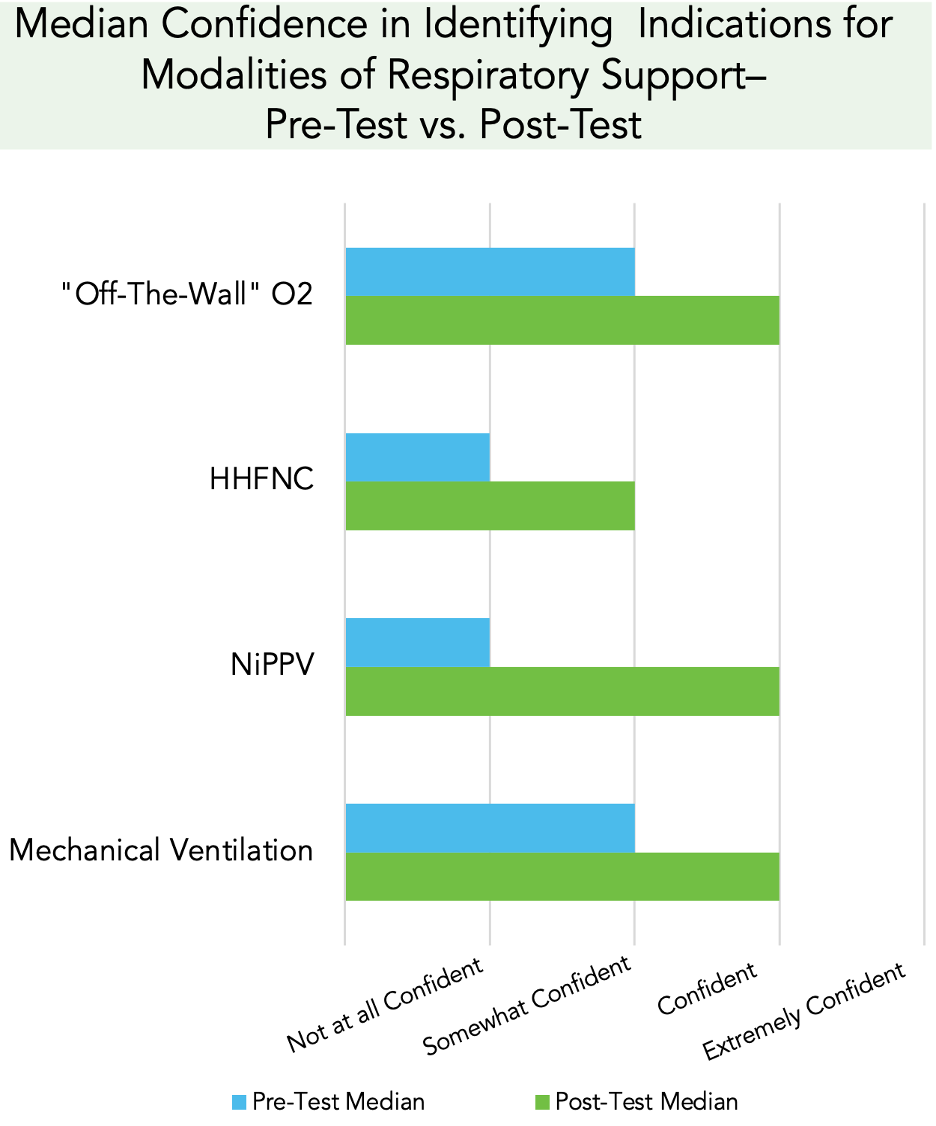
Design/Methods: A novel online module was created using the “EdApp” platform, reviewing commonly encountered types of respiratory support in the clinical setting: supplemental oxygen (O2), heated high flow nasal cannula (HHFNC), non-invasive mechanical ventilation, and invasive mechanical ventilation. Students completed a pre-test survey, the module, and a post-test survey during their clerkship orientation. Both surveys had 3 content-based multiple choice questions and 15 subjective items evaluating confidence in identifying respiratory devices and indications for use. The post-test survey also assessed the effectiveness, difficulty, clinical relevance, and overall quality of the module. Subjective items were measured using a Likert scale.
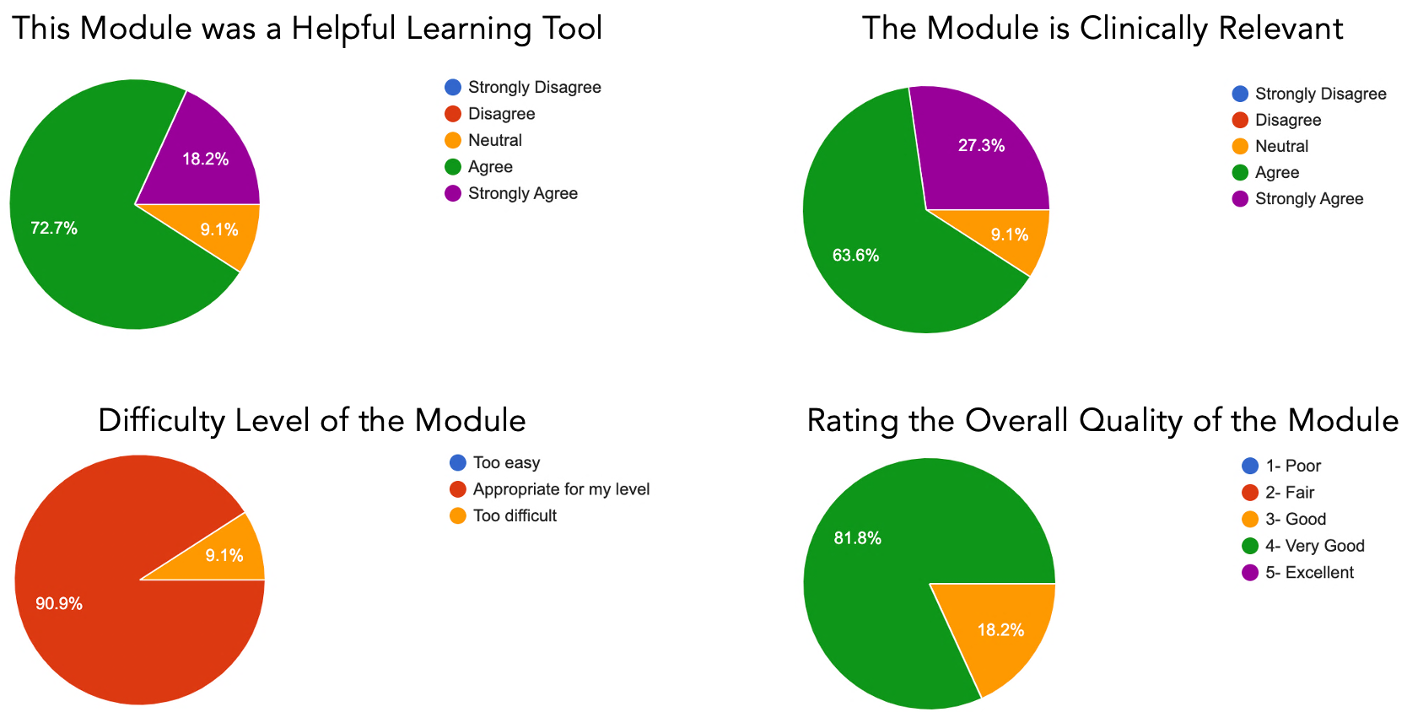
Results: Twenty-three students completed the module and surveys. Paired t-test was used to calculate p-values comparing the pre- and post-test responses, with a p-value < 0.05 being statistically significant. Students scored an average of 28% higher for the post-test multiple choice questions (p < 0.001). Students reported increased confidence in identifying all devices (p < 0.05) except for O2 face masks (p=0.557) on the post-test. Students felt more confident in identifying indications for supplemental O2 (p < 0.001), HHFNC (p < 0.001), non-invasive mechanical ventilation (p < 0.001), and invasive mechanical ventilation (p=0.001) on the post-test. 95.7% of students agreed or strongly agreed that the module was a helpful learning tool, 95.7% indicated that the module was appropriate for their level of learning, 91.3% agreed or strongly agreed that the module was clinically relevant, and the median rating of the module was “very good”.
Conclusion(s): Students had a better understanding of pediatric respiratory support after completing this module. They had increased confidence in identifying a majority of the respiratory devices, and increased confidence in identifying indications for all of the respiratory modalities outlined. Students deemed the module to be a clinically relevant and helpful learning tool and appropriate for their level of learning. Future directions for this project include expansion of respiratory modalities covered.