Neonatology
Session: Neonatal Quality Improvement 6
95 - Standardized Discharge Recommendations for Neonatal Intensive Care Patients: Quality Improvement Initiative
Monday, May 6, 2024
9:30 AM - 11:30 AM ET
Poster Number: 95
Publication Number: 95.3115
Publication Number: 95.3115

Alexandria Martin, MD (she/her/hers)
Resident
Madigan Army Medical Center
University Place, Washington, United States
Presenting Author(s)
Background: There are no national practice guidelines for managing neonatal intensive care unit (NICU) graduates in primary care. Handoffs from the NICU to the outpatient setting is prone to medical errors, wide variability, and suboptimal care ranging from nutrition to appropriate screening. Standardization in patient handoffs reduces medical errors and improves the quality of care.
Objective: Our aim is to create a standardized smart-phrase for all NICU discharge summaries that will increase adherence to evidence-based guidelines for NICU graduates, overall improving the outpatient care.
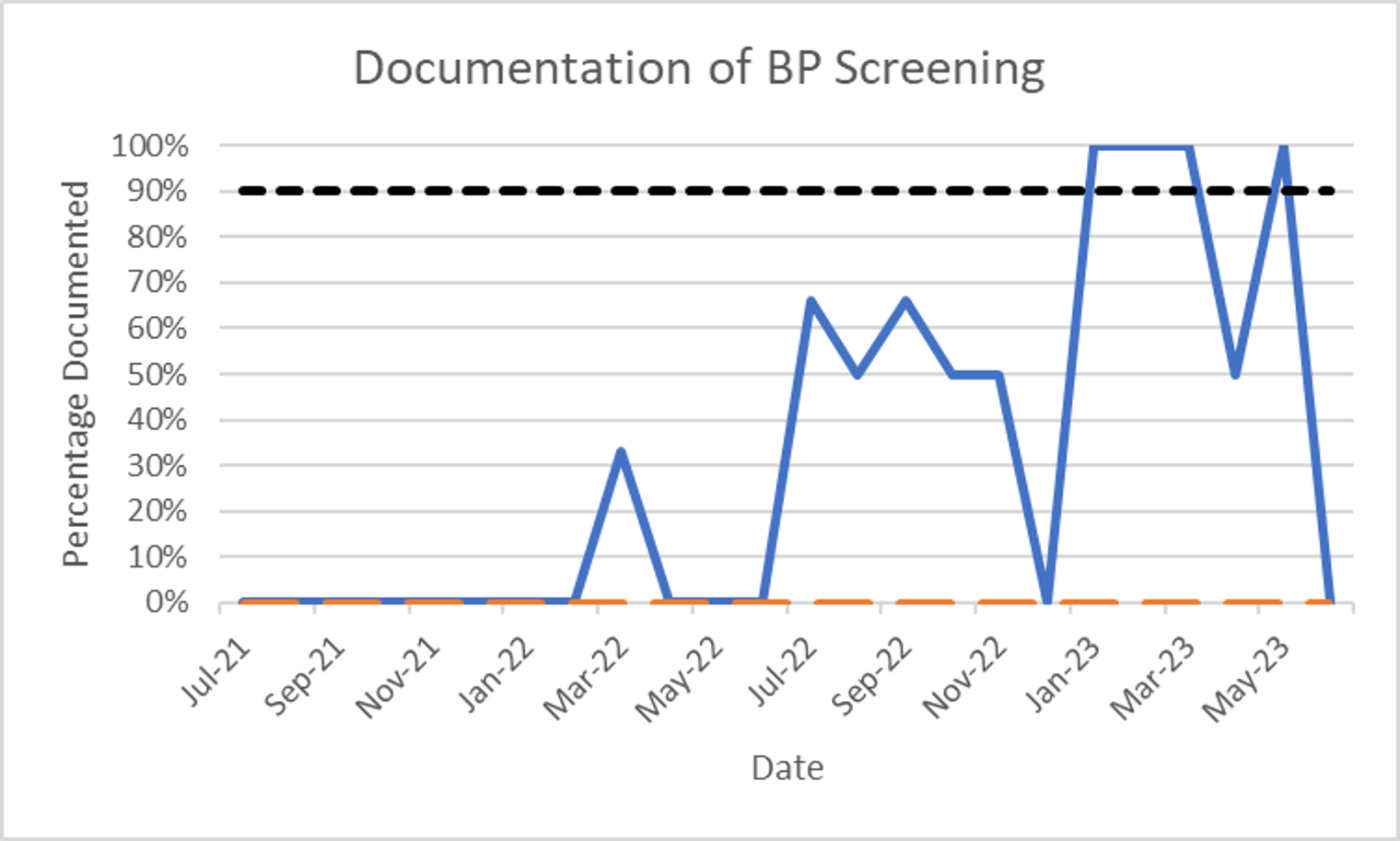
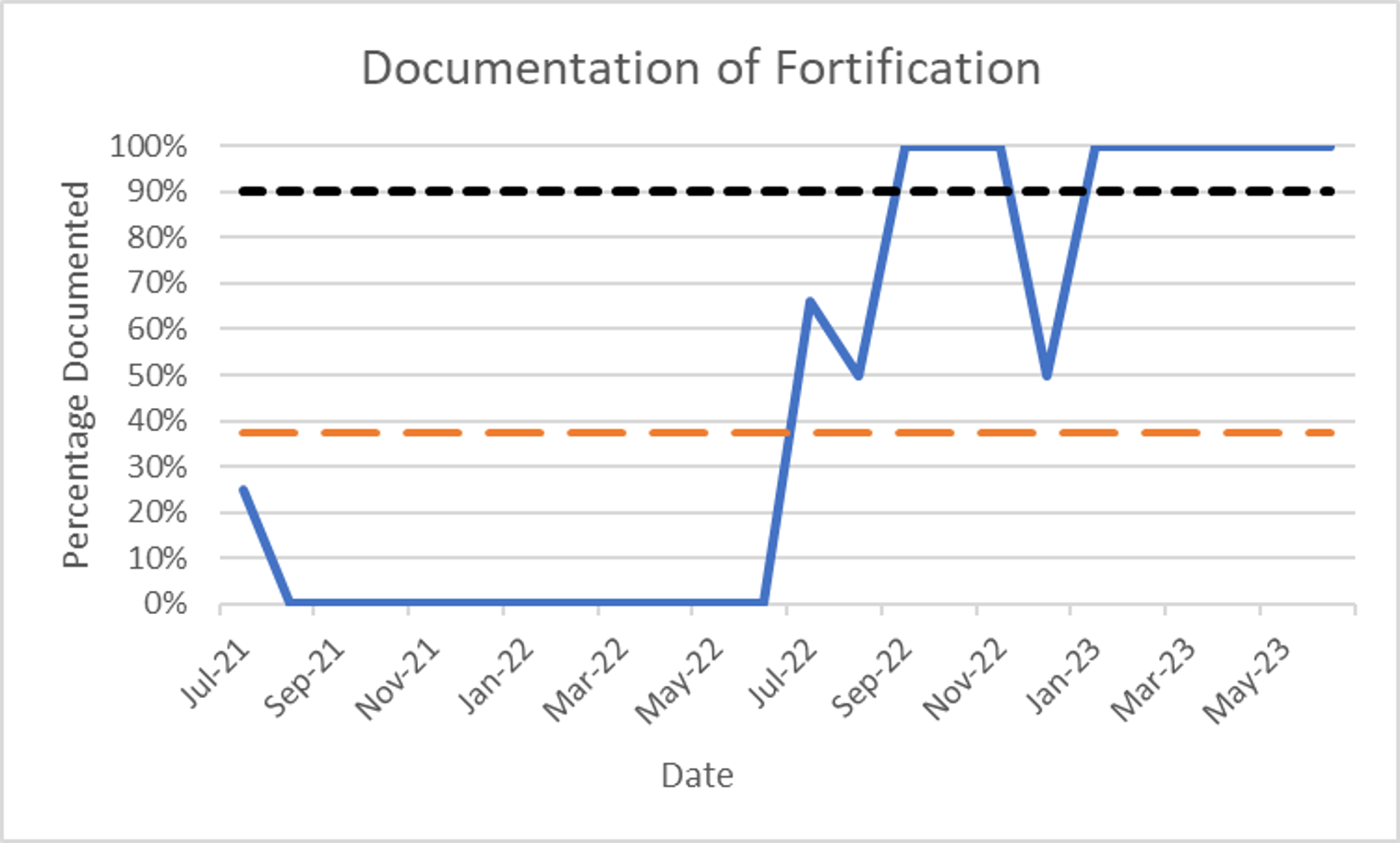
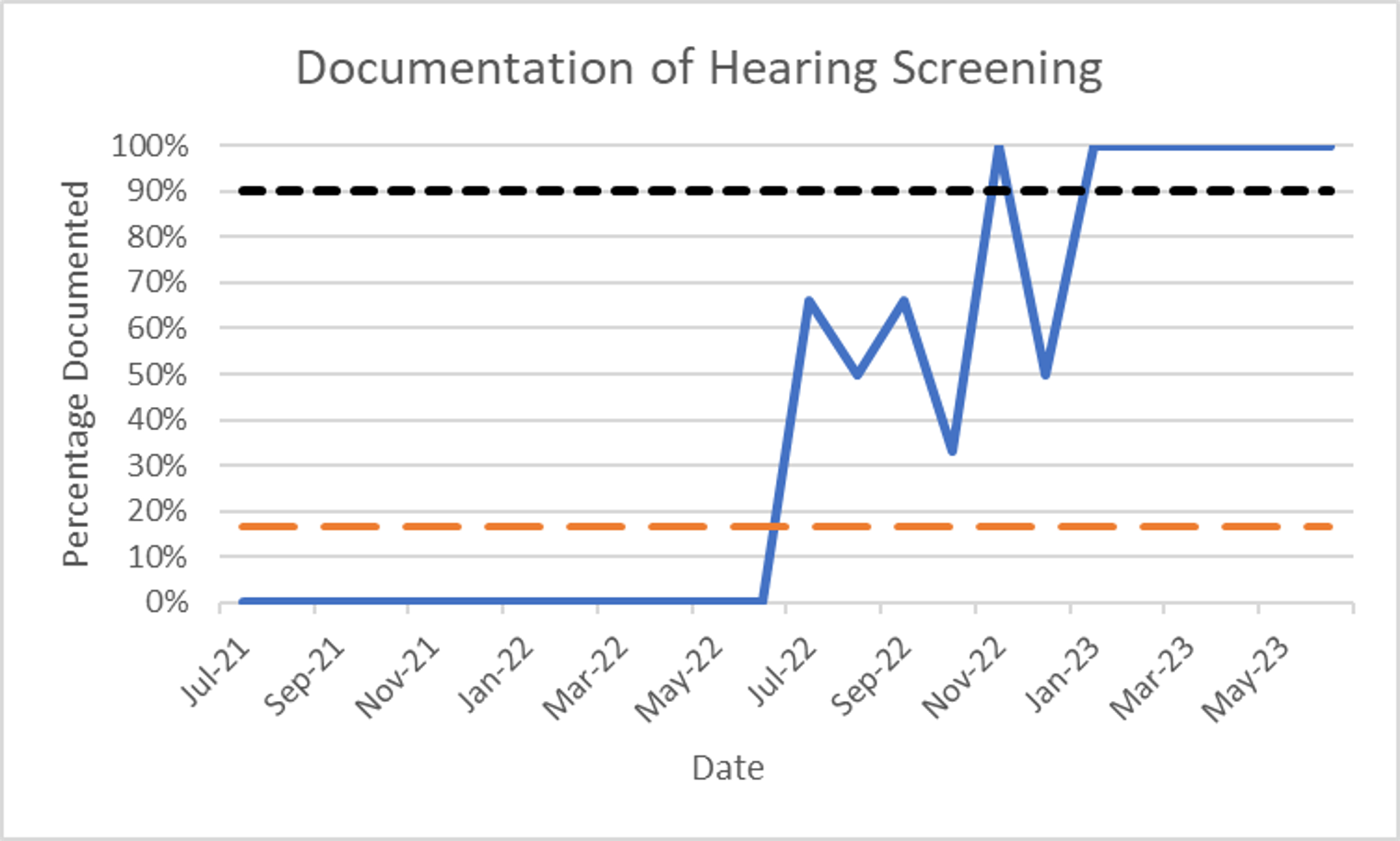
Design/Methods: A single-center retrospective review of the presence of recommendations in NICU discharge notes and outpatient adherence to these recommendations pre-implementation (PRE) and post-implementation (POST) of the standardized smart-phrase was conducted. The project scope includes all infants admitted to the NICU for >5 days and < 35 weeks' gestation discharged one year pre-implementation and one-year post-implementation (July 2021 to June 2023). The project excluded neonates that were not discharged from the NICU due to transfer or death. We created evidence-based health-care maintenance (HCM) recommendations based on a literature review, including audiology screening, hemodynamic monitoring, nutrition with a feeding regimen and length of fortification, and developmental follow-up. A Fischer’s exact test is used to determine the association between implementation of the NICU smart-phrase and documentation of HCM recommendations at time of discharge.
Results: Of 75 neonates within the scope of the research project, 44 charts (59%) were pre-implementation of the smart phrase and 31 charts (41%) post-implementation. Implementation of the standardized smart-phase showed statistically significant improvement in documentation of fortification length (p < 0.001), hearing follow-up (p < 0.001), and blood pressure screening ( < 0.001) in NICU discharge summaries. There was a correlation in implementation of the smart-phrase with placement of an audiology referral at 6 months corrected gestational age (p < 0.001).
Conclusion(s): NICU graduates have medically complex and extended hospital stays that can significantly burden the patient-centered medical home. There is considerable variation in the quantity and quality of discharge documentation on HCM recommendations. With a standardized smart-phrase that included HCM recommendations in discharge summaries, there is statistically significant improvement in recommendations for nutritional guidelines, audiology screening, and routine health maintenance for our NICU patients.